Lancet Neurol:简单可靠的老年痴呆症诊断标准
2014-07-18 佚名 生物通
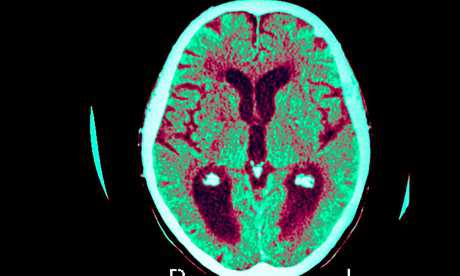
阿尔茨海默氏病(Alzheimer's disease,老年痴呆症)是一种神经退行性疾病,是痴呆最常见的一种类型(70%)。在法国,患有老年痴呆症和其他形式痴呆的人数估计在75万和100万之间,到2030年预计将达到129万到140万之间。老年痴呆症起因于神经元的损失。病变是由一些大脑蛋白的积累引起。病理学始于记忆问题。紧随其后的是时间和空间上的定位问题、行为问题和自主性丧失。然而,这些症状并不是
阿尔茨海默氏病(Alzheimer's disease,老年痴呆症)是一种神经退行性疾病,是痴呆最常见的一种类型(70%)。在法国,患有老年痴呆症和其他形式痴呆的人数估计在75万和100万之间,到2030年预计将达到129万到140万之间。老年痴呆症起因于神经元的损失。病变是由一些大脑蛋白的积累引起。病理学始于记忆问题。紧随其后的是时间和空间上的定位问题、行为问题和自主性丧失。然而,这些症状并不是老年痴呆症所特有的。真正的挑战在于,如何将这种疾病与其他类型的痴呆区分开来,并建立可靠的和尽可能早的诊断方法。
在2005年,由法国国家健康与医学研究院(Inserm)的Bruno Dubois协调的一个国际神经专家小组,重新定义了1984年建立的诊断标准。在此之前,研究人员不得不等待患者死亡,通过检测死亡患者大脑中的病变,来建立一种明确的老年痴呆症诊断方法。在活着的患者中,只能推断疾病的一个概率,仅在后期阶段,才能根据痴呆严重程度的某一临界值来进行诊断。
在2007年,该国际小组打破了这些概念。研究人员介绍了一种新的诊断标准,特别是生物标志物。这些是疾病的真正标签,从最初的症状(前驱期)开始就存在。
这些结果的发表形成了一场革命。Bruno Dubois 称:“根据这些新标准,我们发现,在以前一项基于临床标准的治疗试验中,有36%的患者其实并没有患老年痴呆症。”虽然这种分析只涉及到一小群患者,但是影响很严重。患者没有得到正确的治疗和/或护理。有缺陷的病患选择,可能对新治疗中观察到的疗效缺乏造成了影响。
自2007年以来,已经发表了许多研究。该国际小组决定分析这些文献,为老年痴呆症制订更简单和更可靠的诊断方法。Dubois教授表示:“我们已经走到了路的尽头;我们已经到达了本质,产生了一个国际共识。”今后,老年痴呆症的诊断将依靠“疾病所有阶段的仅仅两个临床生物学标准”。
在很多时候,老年痴呆症的诊断主要是根据提示性的临床图片。随后利用生物标志物进行确认或排除。
关于临床图片,有三种情况:
•典型病例(80-85%的病例):情景记忆障碍(称为海马类型遗忘综合征,即使有线索也很难记住一张单词表);
•非典型病例(15-20%的病例):大脑皮层的后部萎缩或失语,或前额叶脑损伤(会导致行为问题);
•临床前状态:无症状高危(患者没有症状,但是在科学研究期间偶然发现有积极的生物标志物),和症状发生前(具有一个基因突变)。
下面两个生物标志物之一是必需的:
•在脑脊液中(通过腰椎穿刺获得):脑蛋白水平异常(β淀粉样蛋白减少和tau蛋白增加)
•在大脑中(通过PET——正电子放射断层扫描)神经影像:淀粉样蛋白示踪剂的保留升高。
这种更简单和更可靠的诊断方法很重要,主要用于各种研究(临床试验、疾病描述、患者群组的监测等等)。在研究以外,生物标志物的使用,非常昂贵和/或侵入性的,目前仍然限于年轻患者或专家中心的疑难病例。
相关研究结果发表在最近的The Lancet Neurology 杂志。
原始出处:
Dubois B1, Feldman HH2, Jacova C3, Hampel H4, Molinuevo JL5, Blennow K6, DeKosky ST7, Gauthier S8, Selkoe D9, Bateman R10, Cappa S11, Crutch S12, Engelborghs S13, Frisoni GB14, Fox NC15, Galasko D16, Habert MO17, Jicha GA18, Nordberg A19, Pasquier F20, Rabinovici G21, Robert P22, Rowe C23, Salloway S24, Sarazin M25, Epelbaum S4, de Souza LC26, Vellas B27, Visser PJ28, Schneider L29, Stern Y30, Scheltens P31, Cummings JL32.Advancing research diagnostic criteria for Alzheimer's disease: the IWG-2 criteria.Lancet Neurol. 2014 Jun;13(6):614-29. doi: 10.1016/S1474-4422(14)70090-0.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Neurol#
31
#Lancet#
35
#痴呆症#
32
个人觉得就此下定论为时过早
170
对临床科研均有帮助。
98
#诊断标准#
30
这个标准会改变指南?
101