Reg Anesth Pain Med:DNB的预测及其危险因素
2015-08-15 张森 译 MedSci原创
困难椎管内阻滞可能与麻醉并发症的发生相关。在进行硬膜外麻醉,腰麻或者腰-硬联合阻滞时,解剖、技术、药理学因素以及对三维空间的认识都可能成为麻醉医生要面临的挑战。预判DNB(A difficult neuraxial block)的能力也许可以使麻醉医生提前采取预防措施规避相关并发症。识别脊髓标志、腰椎影像学表现、肥胖、皮肤到蛛网膜下的距离、硬膜外空间的能力,有助于对D
困难椎管内阻滞可能与麻醉并发症的发生相关。在进行硬膜外麻醉,腰麻或者腰-硬联合阻滞时,解剖、技术、药理学因素以及对三维空间的认识都可能成为麻醉医生要面临的挑战。预判DNB(A difficult neuraxial block)的能力也许可以使麻醉医生提前采取预防措施规避相关并发症。识别脊髓标志、腰椎影像学表现、肥胖、皮肤到蛛网膜下的距离、硬膜外空间的能力,有助于对DNB进行预测。本研究旨在评价DNB的发病率,评估与患者及组织因素相关的DNB,评价预测DNB的累积的风险评分的诊断准确性。
共有73579位患者纳入本次连续队列研究。预定义的DNB分数和患者及组织因素相关的信息也包括与分析之中。使用逻辑回归分析对数据进行处理。我们评价了DNB的与患者相关的风险因素的累计加权比分的诊断准确性。

DNB以及被迫放弃椎管阻滞的发生率分别为3.9(95% 置信区间[95%CI],3.7–4.0)和 0.2(95%CI,0.16–0.22)。BMI(体质指数)≥35及之前出现过DNB与DNB的相关性分别为 3.23 (95% CI, 2.87–3.65) 和 2.00 (95% CI,1.33–3.00)。然而,剩下的与患者相关的协变量与DNB的相关性为实质性较低的比值比。累计总分的诊断准确性表明曲线下的面积为0.62 (95%CI,0.61–0.64),阳性预测值为5%,阳性似然比为1.4。
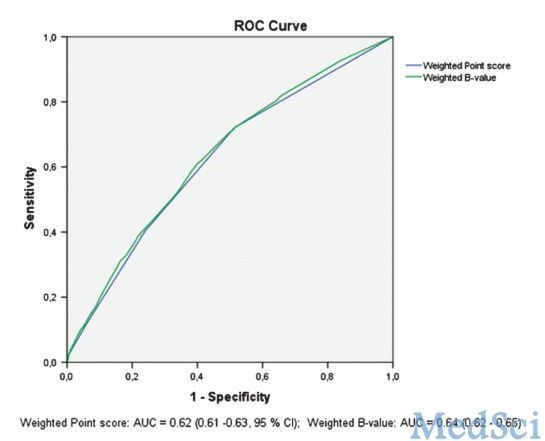
本研究表明:尽管DNB与测试的危险因素间有显著的相关性,低比值比及诊断测试的评估表明使用累计风险总分的临床意义是有限的。
原始出处:
Line Stendell,Lars H. Lundstrøm,Jørn Wetterslev,Theis S.Itenov,and Charlotte V.Rosenstock. Risk Factors for and Prediction of a Difficult Neuraxial Block A Cohort Study of 73,579 Patients from the Danish Anaesthesia Database. Reg Anesth Pain Med. 2015 Jul 31.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








文章不错,值得拜读
50
#EST#
27
#Med#
33