Neurology:Case report:脑脊液过度分流致可逆性执行障碍综合征一例
2022-08-04 Naomi MedSci原创
正常压力性脑积水是一种可逆性的神经疾患。近日,一则发表在Neurology上的Case report报道了一例由脑室-腹腔分流术导致的正常压力性脑积水患者。
近日,一则发表在Neurology上的Case report报道了一例由脑脊液过度分流导致的正常压力性脑积水。
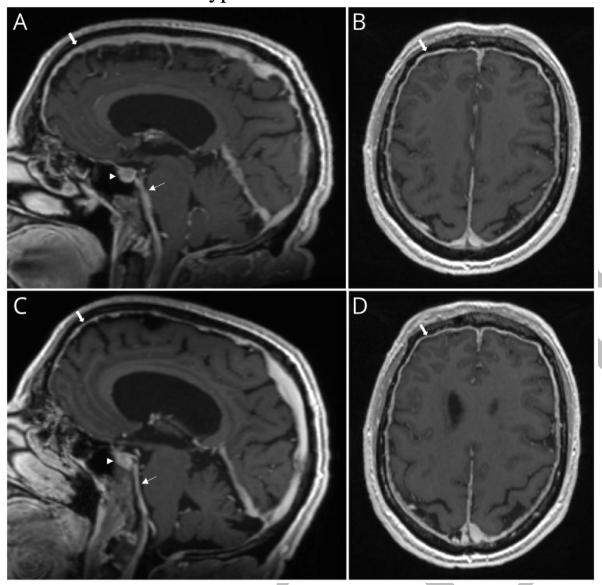
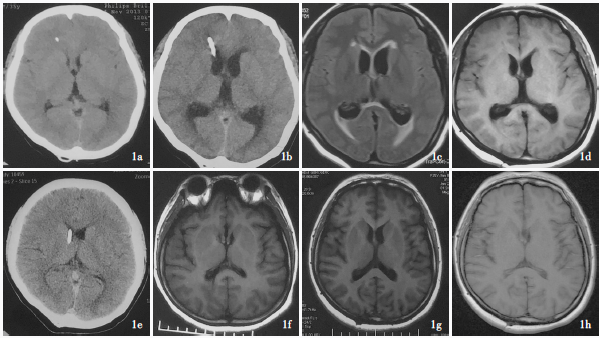
一位72岁的男性科学教师在6次脑室-腹腔分流术后1年出现正常压力性脑积水,伴有颈部疼痛、行为改变和非遗忘性认知下降。6个月前,他的分流术从4变成了3。MoCA 为21/30,其中88个为异常执行优势。脑电图没有异常。脑脊液 AD 生物标志物处于临界状态。MRI 89[图1]发现过度分流。经过分流调整(3-4) ,他的认知和行为90症状得到缓解。4个月后重复 MoCA 为29/30,1年后持续缓解。颅内低压,无论是 VP 分流还是自发性脑脊液漏(1,2) ,都可能引起可逆性执行障碍性认知障碍。
在双侧额叶上方,反映了颅内压低。一年随访MRI C)显示桥脑前池(细箭头)的正常化,垂体窝凸缘(箭头)的减少和双侧额叶上方的硬脑膜增强(箭头) D)的减少,表明进行性分辨的柱头相关的颅内低压。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#case#
50
#Neurol#
51
#case report#
51
?
46
#综合征#
41
#可逆性#
30
#Cas#
44