Cell:对于这种“无药可治”的癌症突变,华人科学家或许找到了解决方案
2018-01-26 佚名 药明康德
在癌症研究领域,KRAS是最为知名的致癌基因之一:科学家们早就发现,在多种人类癌症里,这个基因都发生了突变。然而几十年来,经过数代研发人员的不懈努力,我们依然没有一款能够针对这个基因突变的有效分子。因此,KRAS突变也一度被业内认为是“无药可治”。
今天,发表在顶尖学术刊物《细胞》上的一项研究有望让这一论断成为历史:Wellspring的共同创始人兼首席科学家刘异博士和任平达博士领衔的研究团队发现,一款叫做ARS-1620的分子在体内模型中能选择性地靶向常见KRAS突变,抑制肿瘤生长。如果这款新药能在临床试验中进一步证明自己的潜力,无疑是广大癌症患者的一大福音!
在介绍这项研究前,我们先来看看KRAS基因。先前的研究表明,将近一半的KRAS基因突变为KRAS G12C,即其第12号密码子发生了错义突变(missense mutation)。这个突变能让KRAS蛋白变得过度活跃,导致下游的信号通路异常激活,诱发癌症。据统计,有11%-16%的肺腺癌病例中存在KRAS G12C突变。这一比例在胰腺癌和结直肠癌中则约为1%-4%。
尽管这一KRAS突变带来了极大的医疗负担,但人们却一直没有找到合适的分子,来有效针对这一突变。仅有的几次尝试,也无法在体内模型中彰显其抑制能力。
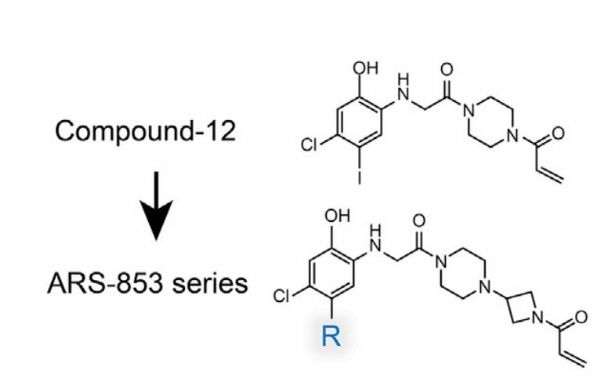
2016年,多个研究团队在针对KRAS突变的小分子抑制剂开发上取得了突破。他们发现,在细胞模型中,ARS-853及其类似物能够与结合了GDP的KRAS G12C突变蛋白产生共价作用,让它转变为“失活”的构象。这固然让研究人员们看到了曙光,也引申出了下一个不得不回答的问题——这些分子的潜力能在体内模型中得到重复吗?
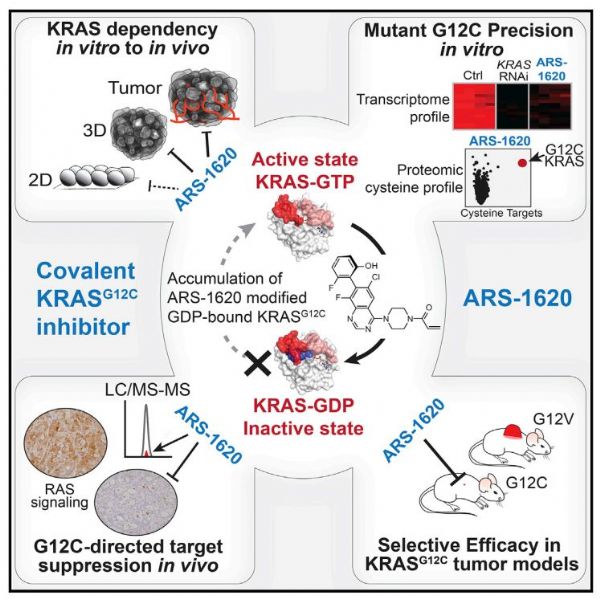
这正是刘异博士团队的成果所在。首先,他们以ARS-853系列分子为基础,重新设计并合成了众多候选分子。这样做的目的在于筛选出最具活性、药代动力学最佳的优化结构。在对这些分子的生化特性与细胞靶点活性进行分析后,一款叫做ARS-1620的分子脱颖而出,它的活性是ARS-853的10倍。
随后,研究人员们分析了ARS-1620的潜在脱靶效应——作为一款共价抑制剂,如果它能显着抑制其他蛋白的功能,就会带来意料之外的副作用。分析表明,KRAS G12C是它最主要的抑制对象。
此外,研究人员们也通过分析全基因组的表达情况,确认了ARS-1620的确可以抑制KRAS的下游通路。
接下来,就是最为令人紧张的时刻了。研究人员们让小鼠模型通过口服摄入了ARS-1620,并分析其该分子在体内的一系列指标。他们高兴地看到,这款分子有着极好的生物可利用性(bioavailability),在血液中的浓度也很稳定。在肿瘤附近,ARS-1620也有着较好的峰值浓度。

▲ARS-1620在体内有效减少的KRAS G12C肿瘤的体积(图片来源:《细胞》)
这些出色的属性,能否让ARS-1620在体内起到抑制肿瘤生长的作用呢?研究人员在小鼠的肿瘤模型中进一步测试了ARS-1620的效果,而结果让人感到欣喜!在两个不同的浓度下,ARS-1620都能显着缩小KRAS G12C肿瘤的体积,而且缩小的幅度与用药量相关。此外,另一种KRAS突变(KRAS G12V)的肿瘤则没有受该分子的影响,体现了该分子的特异性。
在多个KRAS G12C肿瘤模型中,研究人员们成功重复了这一结果——ARS-1620在体内实验中均能显着缩小肿瘤的体积,且彰显出了良好的选择性。
“这些小鼠体内实验的数据表明,ARS-1620在多个模型中都具有疗效。这有望转化为新的疗法,造福那些罹患KRAS G12C的癌症患者,”该研究的通讯作者刘异博士说道:“我感谢参与这项研究的所有科研人员。他们的智慧与努力让这项突破成为了可能。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#解决方案#
38
#CEL#
40
#Cell#
30
学习了.谢谢作者分享!
62
#华人#
35
学习了.涨知识
57