超声心动图双室耦合指数预测毛细血管前肺动脉高压
2022-02-15 刘少飞 MedSci原创
右心导管 (RHC) 是识别 PH 亚型,基于右心室卒中做功指数与左心室 E/E' 比值的新型超声心动图双心室耦合指数 (BCI),以 RHC 作为比较器,测试了对 PH 亚型的区分。
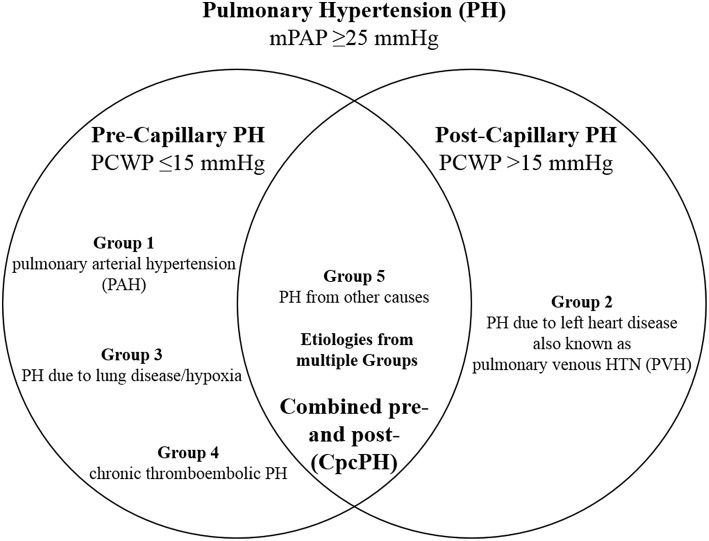
肺动脉高压 (PH) 影响着全世界数百万人。右心导管术 (RHC) 是正确分类 PH 亚型的金标准。双心室耦合指数 (BCI) 是一种新的超声心动图指标,定义为无创右心室卒中功指数 (RVSWI) 与 E/E' 比值之比。由于他对右心生理的全面功能表征,我们假设它可能正确识别毛细血管前 PH。
研究方法:来自于来自的里雅斯特大学医院(意大利)和卡罗林斯卡大学医院(瑞典)的 334 名患者队列,这些患者接受了经胸超声心动图和 RHC 的所有适应症(两次检查之间小于 6 小时)。然后在 1349 名患者的验证队列中测试 BCI。
研究结果:在推导队列中,BCI 识别毛细血管前 PH (pPH) 的准确性很高(AUC 0.82,CI 0.78-0.88,p<0.001,最佳切点 1.9)。BCI 在验证队列中也以高准确度确定了 pPH 患者(AUC 0.87,95% CI 0.85-0.89,p<0.001;PH 亚组:AUC 0.91,95%CI 0.89-0.93,p<0.001,临界点 1.9 , 敏感性 82%, 特异性 89%, 阳性预测值 77% 和阴性预测值 92%)。BCI 优于 D'Alto 评分(Z 系数=3.56,区域间差异=0.05;95%CI 0.02-0.07,p<0.001)和超声心动图肺左心房比指数(Z 系数=2.88,区域间差异= 0.02;95%CI 0.01-0.04,p=0.004)。
研究结论:BCI 是一种基于标准超声心动图参数的新型非侵入性指标,能够以高准确度识别毛细血管前 PH 患者,优于先前提出的指标。BCI 指数的常规使用可用于毛细血管前 PH 的筛选工作。
研究启示:BCI是一种可以正确识别毛细血管前PH值的新指标;BCI 可以减少不必要的右心导管检查。
参考文献:
Albani S. Echocardiographic Biventricular Coupling Index to Predict Pre-Capillary Pulmonary Hypertension. J Am Soc Echocardiogr. 2022 Feb 11:S0894-7317(22)00061-X. doi: 10.1016/j.echo.2022.02.003. Epub ahead of print. PMID: 35158052.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#动脉高压#
29
#心动图#
54
#超声心动图#与#肺动脉高压#
119
#毛细血管#
37