HEPATOLOGY:上海药物所揭示 pIgR/p-Yes 亚群分型是肝癌患者生存的预后标志物
2017-03-31 佚名 上海药物研究所
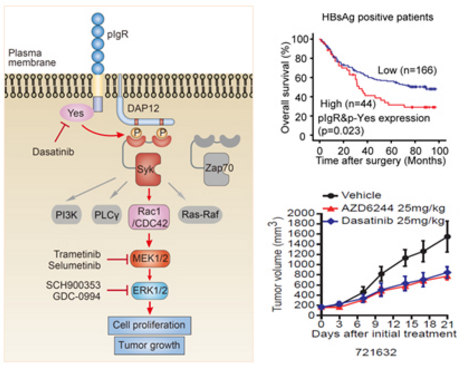
高表达 pIgR 体内外显著促进肝癌细胞恶性增殖和肿瘤生长。分子机制研究表明,介导 pIgR 免疫转运的关键激酶 Yes 参与调控了 pIgR 介导的肿瘤生长效应;深入机制研究发现,pIgR 通过募集活化 Yes,启动了基于 ITAM 基序的经典免疫受体相关通路介导肿瘤生长。
pIgR 通常感受炎性微环境调控,介导细胞内多聚免疫球蛋白 IgA 和 IgM 的极性转运,是粘膜上皮组织最为重要的一个连接天然免疫和获得性免疫的免疫球蛋白受体。中国科学院上海药物研究所的科研人员在前期工作中首次发现了 pIgR 感受炎性微环境上调,通过募集活化 Smad 复合物,显着诱导肝癌细胞的上皮细胞间充质转化(EMT),促进肝癌的早期复发与转移(J Natl Cancer Inst. 2011;103(22):1696-712)。
经科研人员近期的研究表明,高表达 pIgR 体内外显着促进肝癌细胞恶性增殖和肿瘤生长。分子机制研究表明,介导 pIgR 免疫转运的关键激酶 Yes 参与调控了 pIgR 介导的肿瘤生长效应;深入机制研究发现,pIgR 通过募集活化 Yes,启动了基于 ITAM 基序的经典免疫受体相关通路介导肿瘤生长。上海药物所耿美玉课题组、丁健课题组在此基础上进一步与复旦大学附属中山医院合作,在对 254 例肝癌临床组织样本分析后发现,pIgR/p-Yes 这个亚群是肝癌预后不良的重要预测标志物,在 HBV 阳性及早期病人中意义尤为显着;pIgR/p-Yes 双阳性是肝癌总存活、总复发的独立预后标志物,对肝癌早期诊断具有重要的指导意义。更为重要的是,科研人员采用已上市药物,对于 pIgR/p-Yes 这个亚群提出了针对性的靶向治疗策略(Dasatinib/MEK 抑制剂),并在肝癌病人来源的 PDX 模型研究中进行了验证,Dasatinib/MEK 抑制剂可以显着抑制 pIgR/p-Yes 双阳性亚群的肿瘤生长。
该研究挑战了对 pIgR 传统功能认识的局限,为免疫球蛋白受体的两面性提供了重要范例。pIgR 采用生理条件下免疫转运相关通路介导肿瘤细胞恶性生长,为 pIgR 免疫背叛的深入理解奠定了基础。同时,研究工作也有效拓展了 Dasatinib、MEK 抑制剂的新敏感群体,对该类药物的临床应用具有重要的指导意义。
研究成果于 1 月 10 日在线发表于 Hepatology。研究工作得到了国家自然科学基金委、科技部、中科院战略性先导科技专项等有关项目的资助。
原始出处:
Xihua Yue, Jing Ai, Yang Xu, et al. Polymeric immunoglobulin receptor promotes tumor growth in hepatocellular carcinoma. Hepatology, 10 January 2017. DOI: 10.1002/hep.29036.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#患者生存#
28
#标志物#
36
#上海药物所#
37
#预后标志#
49
#肝癌患者#
30
谢谢分享。学习
45
好好学习
52
文章不错,值得分享
47
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。
54
#EPA#
28