JCO:35岁以下乳腺癌患者:辅助内分泌治疗是把双刃剑?
2017-07-02 陶白 肿瘤资讯
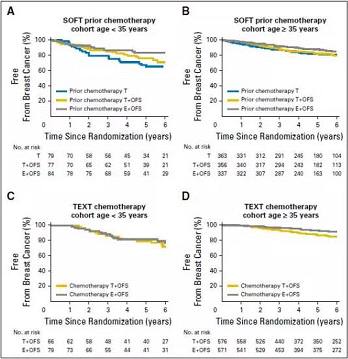
<35岁的乳腺癌患者面临局部和远端复发的风险。辅助内分泌治疗可延长5年无乳腺癌间期,但会使症状特异性生活质量变差。如何权衡辅助内分泌治疗的风险和获益?其在不同年龄组中是否具有差异?6月27日JCO上在线发表一项研究对此进行了分析。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCO#
25
#分泌#
37
文章不错,谢谢分享
53
文章很好,拜读了
68
#乳腺癌患者#
29
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
1
学习了。。。
52
学习了,谢谢分享
48
乳腺癌研究好好
30
好好的学习一下
29