Cell Death Differ:TBC1D17-Rab5通路影响2型糖尿病相关的葡萄糖摄取
2021-05-28 xiaozeng MedSci原创
2型糖尿病是一种与年龄相关的疾病,其在全球范围内影响着超过400万人。
2型糖尿病是一种与年龄相关的疾病,其在全球范围内影响着超过400万人。作为该疾病的主要特征,胰岛素抵抗会导致葡萄糖稳态的失调。
既往研究显示,Glut1(葡萄糖转运蛋白1)的表达下调和胰岛素反应性Glut4的转运受损均会促进胰岛素抵抗作用的发生。除胰岛素外,运动是骨骼肌中Glut4转运的另一种重要的生理刺激。AMP和ADP含量的增加会激活细胞中的能量传感器AMPK(AMP活化激酶),并随后介导运动/肌肉收缩对葡萄糖摄取的影响,然而其潜在的分子机制尚不清楚。
因此,进一步的了解AMPK介导的信号转导通路可为治疗与2型糖尿病相关的胰岛素抵抗提供新的见解和潜在的治疗靶标。
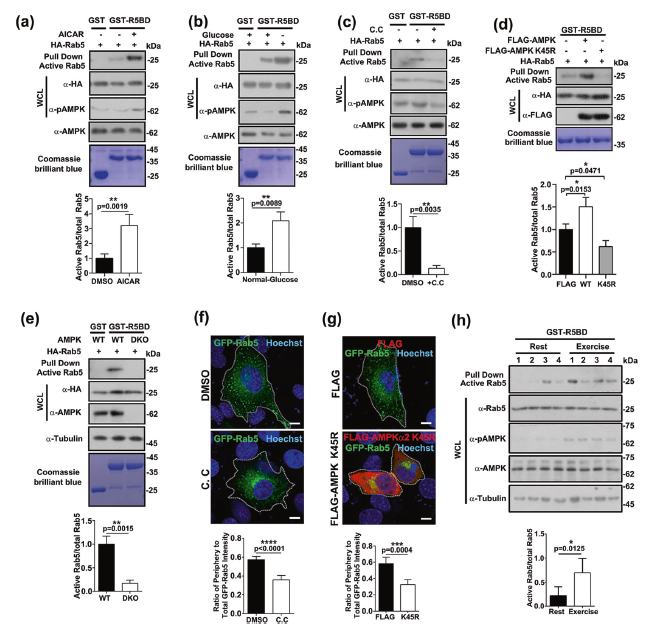
在该研究中,研究人员发现,在骨骼肌和成肌细胞中AMPK均能够正调控Rab5的激活。Rab5是一种小的GTP酶,是核内体融合、转运和生物发生的重要调节因子,其参与调节Glut4的转运。
AMPK激活Rab5
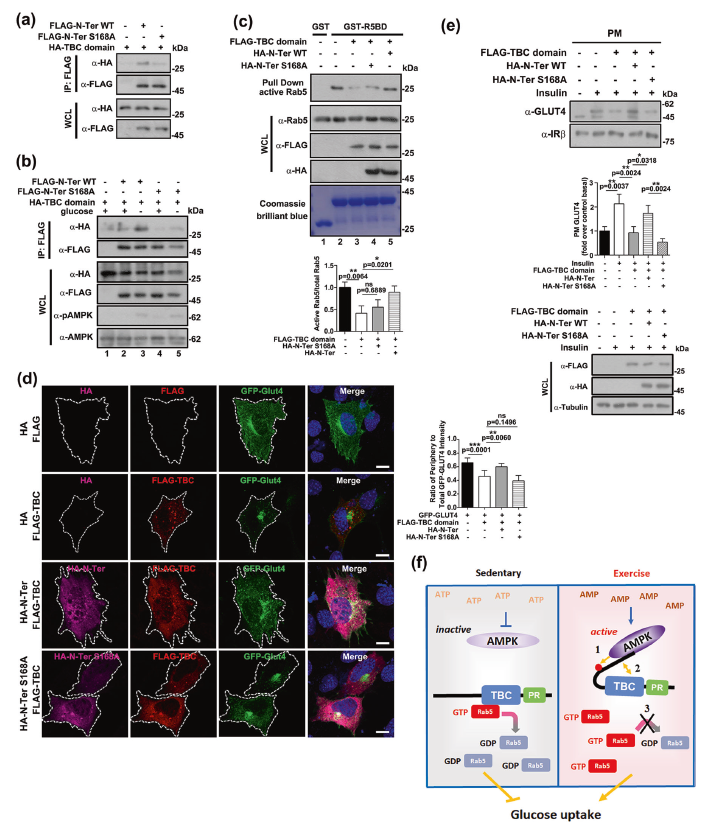
进一步的研究显示,被确定为Rab5潜在相互作用伴侣的TBC1D17是Rab5的新型GTPase激活蛋白(GAP)。TBC1D17-Rab5通路能够调节Glut1、Glut4和转铁蛋白受体的转运。而TBC1D17分别通过其RBC5结构域或N末端1–306区域(N-Ter)与Rab5或AMPK相互作用的。
此外,AMPK能够磷酸化TBC1D17的第168位Ser丝氨酸残基,该残基与预测的AMPK共有基序匹配。TBC1D17的N-Ter结构域能够通过与TBC结构域直接相互作用而充当抑制区。该蛋白的Ser168磷酸化能够促进分子内的相互作用,从而增强TBC1D17的自抑制作用。
Ser168磷酸化增强TBC1D17的自抑制作用
综上,该研究结果表明,TBC1D17能够充当连接AMPK和Rab5的分子桥,并揭示了调节TBC/RabGAP激活的相关分子机制。TBC1D17-Rab5通路或可成为治疗代谢性疾病和衰老的一个潜在的靶标。
原始出处:
Rao, X.S., Cong, X.X., Gao, X.K. et al. AMPK-mediated phosphorylation enhances the auto-inhibition of TBC1D17 to promote Rab5-dependent glucose uptake. Cell Death Differ (27 May 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Cell#
46
#CEL#
44
#Differ#
26
#Death#
43
谢谢MedSci提供最新的资讯
66