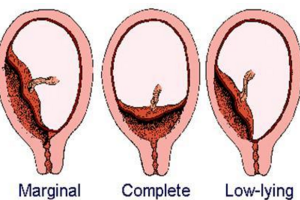
胎盘植入诊治面临的挑战与策略
2016-05-31 贺芳 陈敦金 中国实用妇科与产科杂志
胎盘植入临床处理既有共性又有每位孕产妇的特殊性, 不同处理方式导致其患者结局不一,应引起产科医师的高度重视。 作者:贺芳 陈敦金(广州医科大学附属第三医院) 来源:《中国实用妇科与产科杂志》 摘要:胎盘植入可导致严重的产时出血,造成母亲产后出血,出血性休克,子宫切除,组织器官缺血再灌注损伤乃至孕产妇死亡,以及胎儿医源性早产发病率和死亡率升高。胎盘植入的处理策略是合理的期待
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#胎盘植入#
43
#胎盘植入#
47
#胎盘#
0
#植入#
31
学海无涯!
163
学习学习!
127
远高于发达国家,任重道远
92