Allergy:嗜酸细胞状态不影响Dupilumab的慢性鼻窦炎伴鼻息肉疗效
2021-06-20 AlexYang MedSci原创
慢性鼻窦炎伴鼻息肉(CRSwNP)是一种鼻腔和副鼻窦慢性炎症性疾病,与较大的症状负担和健康相关的生活质量(HRQoL)有关。CRSwNP病理生理学的主要特点是2型炎症,白细胞介素(IL)-4、IL-1
慢性鼻窦炎伴鼻息肉(CRSwNP)是一种鼻腔和副鼻窦慢性炎症性疾病,与较大的症状负担和健康相关的生活质量(HRQoL)有关。CRSwNP病理生理学的主要特点是2型炎症,白细胞介素(IL)-4、IL-13和IL-5是优势细胞因子,以及嗜酸细胞、淋巴细胞、嗜碱细胞和肥大细胞的组织浸润。

人类单克隆抗体dupilumab能够阻断白细胞介素(IL)-4和IL-13,这两者是2型炎症的关键和核心驱动因素。在III期SINUS-52研究(NCT02898454)中,Dupilumab在糠酸莫米松鼻喷雾剂(MFNS)的基础上,改善了伴有鼻息肉的严重慢性鼻炎(CRSwNP)患者的治疗效果。近期,研究人员对SINUS-52进行了事后分析,考察了CRSwNP的嗜酸细胞状态是否是预测dupilumab疗效的一个预测因子。
研究人员将患者按1:1:1的比例随机接受dupilumab 300mg,每2周(q2w)一次,共52周;dupilumab 300mg q2w,共24周,然后每4周300mg,直至第52周;安慰剂(MFNS),共52周。终点是第24周时鼻息肉评分(NPS)、鼻塞(NC)和CT评估的Lund-Mackay评分(LMK-CT)与基线相比的变化。
研究共包括了438名患者,在所有ECRS亚组中,与安慰剂相比,Dupilumab在第24周明显改善了NPS、NC和LMK-CT评分(P<0.001),在第52周改善情况得以保持或增强(P<0.001)。在第24周和第52周,ECRS亚组(非/轻度或中度/重度)与dupilumab治疗效果之间没有明显的交互作用(p>0.05),除了第24周的LMK-CT(p=0.0275)。次要终点也有类似的结果。另外,Dupilumab在所有ECRS亚组中的耐受性良好。

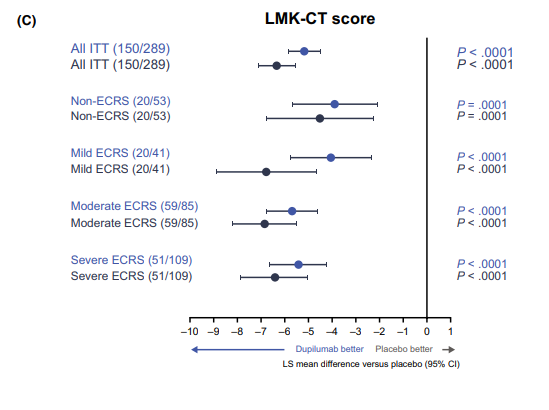
Dupilumab 300mg与安慰剂对第24周和52周症状评分的影响
综上所述,无论ECRS状态如何,Dupilumab对重度CRSwNP症状产生了一致的改善。因此,血液中的嗜酸性粒细胞水平可能不是衡量dupilumab对CRSwNP疗效的合适生物标志物。
原始出处:
Shigeharu Fujieda , Shoji Matsune , Sachio Takeno et al. Dupilumab efficacy in chronic rhinosinusitis with nasal polyps from SINUS-52 is unaffected by eosinophilic status. Allergy. May 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#mAb#
46
#Dupilumab#
50
#ALL#
0
#慢性鼻窦炎#
59
😏
72
谢谢梅斯提供这么好的信息,学到很多
60