Circulation: LDL-C降至婴儿水平,可进一步降低心血管病风险
2016-12-31 中国中医科学院西苑医院心血管病中心 李圣耀 医学界心血管频道
将LDL-C进一步降低到50mg/dL(1.3mmol/L)以下,几乎是刚出生的婴儿水平,是否还能进一步获益?其安全性如何?是临床医生普遍关心的问题。《Circulation》上刊登的最新研究再次印证了LDL-C持续降低,甚至低于50mg/dL,与MACE降低的一致性关系。LDL-C水平降到多少合适,一直被热烈争论:基于他汀常规治疗和强化治疗的临床研究,ATP III、ESC/EAS指南推荐动脉粥
将LDL-C进一步降低到50mg/dL(1.3mmol/L)以下,几乎是刚出生的婴儿水平,是否还能进一步获益?其安全性如何?是临床医生普遍关心的问题。
《Circulation》上刊登的最新研究再次印证了LDL-C持续降低,甚至低于50mg/dL,与MACE降低的一致性关系。
LDL-C水平降到多少合适,一直被热烈争论:基于他汀常规治疗和强化治疗的临床研究,ATP III、ESC/EAS指南推荐动脉粥样硬化高危患者LDL-C应降至70 mg/dL以下;随后,ACC/AHA和NICE指南提出不设定LDL-C的目标值,认为对于高危患者来说LDL-C应至少降低30-50%。
但对于使用最大耐受量的他汀将LDL-C将至70 mg/dL以下或更大的降幅,能否带来MACE事件的进一步降低仍然不确定,直到IMPROVE-IT研究给我们带来非他汀类药物获益的证据:该研究显示依折麦布联合他汀可将LDL-C降至54 mg/dL左右,且能进一步降低MACE事件。这再次印证了"胆固醇学说"的正确性,即MACE事件的降低,得益于LDL-C的降低,而不是他汀药物本身。同时该研究还支持,在70 mg/dL基础上,LDL-C再降低20%,还可以带来MACE事件6-7%的降幅。
《Circulation》上刊登的这篇文章,作者汇总了10项研究,这些研究的目的是观察在最大耐受量的他汀治疗基础上,与安慰剂或依折麦布相比,加用新型降脂药alirocumab是否可进一步降低 LDL-C、非-HDL-C和载脂蛋白B100水平,MACE事件是否进一步减少。该研究共包括了4974名患者(3182名服用alirocumab,1174名服用安慰剂,618名服用依折麦布)。
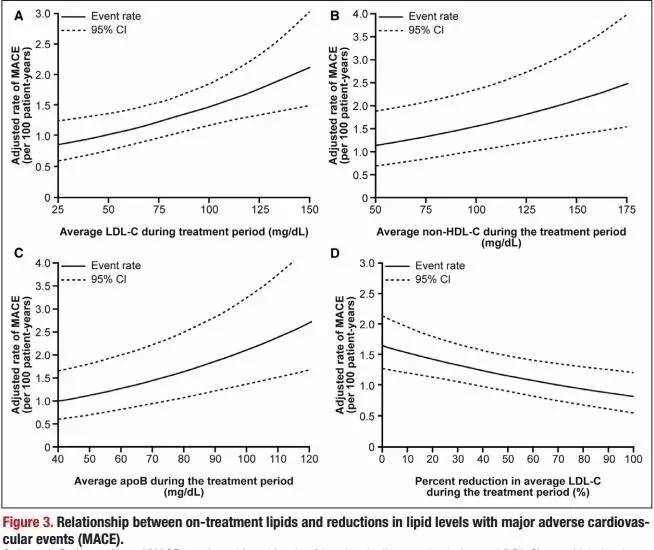
结果发现,33.1%的队列LDL-C水平降至低于50 mg/dL的水平(44.7%-52.6%的患者服用alirocumab,6.5%服用依折麦布,0%服用安慰剂),有104位患者发生了MACE事件(发生事件的中位时间为36周)。在他汀最大耐受量基础上,LDL-C每降低39 mg/dL(1.0 mmol/L),MACE事件的风险进一步降低24%(调整风险比0.76,95%可信区间,0.63-0.91;P=0.0025)。这与胆固醇治疗试验(CTT)的meta回归线预测的22%的结果相当接近。
尽管强化他汀治疗已可带来LDL-C近50%的降幅,但合并PCSK9抑制剂后,可在此基础上再降50-60%,相当于与基线相比的75-80%的降幅,且LDL-C降幅越大,MACE事件风险越低(RR,0.71;95%可信区间,0.57-0.89,与基线相比每降低50%)。非-HDL和载脂蛋白B100治疗后的水平及降幅,也与MACE事件风险的下降相关,结果与LDL-C相似。在观察期间,与治疗相关的副作用并没有增加。
这一研究表明,LDL-C更大的降幅,更低的水平(甚至<50mg/dL),可进一步降低MACE事件(冠心病死亡、非致死性心肌梗死、缺血性中风或需住院治疗的不稳定型心绞痛)发生率,且安全性良好。目前,在最大耐受量的他汀基础上,加用PCSK9抑制剂alirocumab,能否进一步降低MACE事件的随机对照研究如ODYSSEY OTUCOMES正在进行中。如果这些试验证实LDL-C进一步降低的临床获益,指南将有可能改写:对于MACE事件的高风险人群,LDL-C应降至更低的水平,更大的降幅。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血管病#
44
谢谢分享,学习了
82
很好,不错,以后会多学习
86
#LDL#
35
谢谢,有作用的
0