JNNP:脑肿瘤患者观看电影时的功能磁共振成像用于术前语言检查
2021-07-11 MedSci原创 MedSci原创
术前语言检查的主要目标是定位具有高度敏感性(即捕捉切除可能导致语言缺陷的区域)和特异性(即排除非语言区域)的关键语言区域,并在个体基础上可靠地确定语言半球优势。由于语言在额叶、颞叶和顶叶广泛分布的功能
术前语言检查的主要目标是定位具有高度敏感性(即捕捉切除可能导致语言缺陷的区域)和特异性(即排除非语言区域)的关键语言区域,并在个体基础上可靠地确定语言半球优势。由于语言在额叶、颞叶和顶叶广泛分布的功能组织,以及在神经外科患者中肿瘤引起的功能重组的可能性,语言检测具有挑战性。传统的基于任务的功能性磁共振成像(tb-fMRI)被推荐用于术前语言检测的一个主要缺点是患者执行精确定时任务的偶然性。无任务静息态功能磁共振成像(rs-fMRI)的缺点包括“心不在焉”的混淆效应和对运动伪影的敏感性。与此相反,电影观看是一种丰富的、刺激的、自然的活动,它可以在现实生活中约束认知过程,参与支持语言功能的分布式、多模态的神经网络。之前的研究表明,在神经健康受试者中使用电影观看功能磁共振成像(mw-fMRI)进行个体语言区域检测。本文研究了脑肿瘤侵犯假定语言皮质和不同程度语言中断的术前患者的mw-fMRI语言检测。

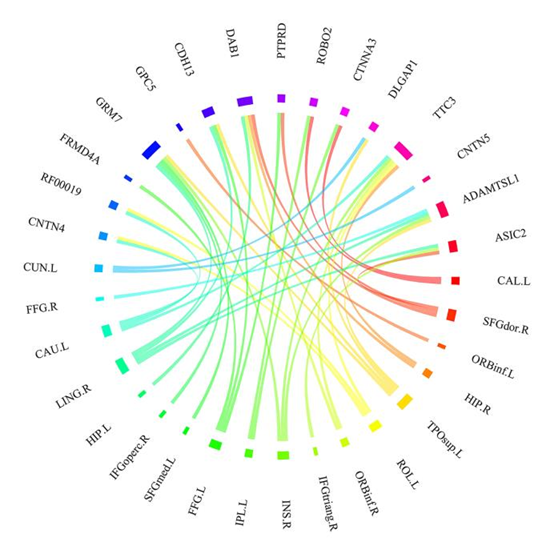
对34例接受术前语言检查的脑瘤患者进行Mw-fMRI与临床的AntGen-tb-fMRI比较,其中22例与rs-fMRI比较。用线性模型从tb-fMRI和mw-fMRI及rs-fMRI生成语言图。对于mw功能磁共振成像,主要和次要的语言成分(LC1,LC2)具有不同的时间进程,通过空间相关性与一个典型的语言模板(包括额叶,颞叶和顶叶皮质区域)进行识别,与来自独立神经健康组的模型时间过程的时间相关性对比。对于rs功能磁共振成像,使用语言模板的空间相关性识别语言成分。以10%的阈值计算每个范式的语言映射度量 。
由于头部过度运动,一名受试者的Mw-fMRI数据(2.9%)、四名受试者的tb-fMRI数据(11.8%)和两名受试者的rs-fMRI数据(9.1%)被排除在分析之外。mw-fMRI比tb-fMRI患者的头部运动范围更低,两种模式之间未发现其他差异。由于在mw-fMRI和rs-fMRI中未能识别语言部分,排除了一名受试者的数据。与tb-fMRI相比,mw-fMRI-LC1对双侧颞叶皮层的敏感性较高,对双侧额叶皮层的敏感性较低;LC2在顶叶皮质的敏感性较高。mw-fMRI-LC1显示出比tb-fMRI更高的特异性。mw-fMRI敏感性与rs-fMRI相当,特异性更高。
基于电影观看(mw-fMRI)、反义词生成(AntGen-tb-fMRI)和静息状态(rs-fMRI)的脑肿瘤患者fMRI语言检测
mw-fMRI和tb-fMRI在顶叶(p=0.039)、颞叶(p=0.063)和额叶(p=0.058)区域的偏侧性存在显著差异。多数不一致病例tb-fMRI表现为左半球优势,mw-fMRI表现为右半球优势。mw-fMRI与rs-fMRI无差异。mw-fMRI与tb-fMRI和rs-fMRI相比具有更高的语言检测特异性,表明在假定的语言区域之外,假阳性激活的发生率较低。实际上,更高的特异性会有利于神经外科肿瘤切除。AntGen范式的低特异性可能是由于任务与对照条件下视觉区域的更大激活,说明tb-fMRI依赖于基线的选择。

语言检测的高灵敏度表明在假定的语言区域内假阴性激活的发生率较低,这一点很重要,因为它可以降低手术后语言缺陷的风险,这与低估和意外切除功能组织有关。目前的研究结果表明,mw-fMRI可能在颞叶和顶叶皮质提供更高的检测敏感性,主要与接受性语言功能有关,而在额叶区则提供较低的标测敏感性,主要与表达性语言功能有关。这一发现与先前的研究结果一致,即语音要求任务特别涉及背听语音流和额叶皮层,而看电影则涉及广泛的颞顶语义网络。Mw-fMRI与rs-fMRI表现出良好的偏侧一致性,但与tb-fMRI有一定程度的差异。
mw-fMRI可以作为颞顶叶病变患者tb-fMRI的补充或替代方法,对这些患者来说,高精度的颞顶叶病变区术前标测是必不可少的,任务执行可能具有挑战性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#功能磁共振成像#
29
#磁共振#
30
#脑肿瘤#
35
#语言#
42
#肿瘤患者#
35
#功能磁共振#
41
#功能MRI#功能核磁很值得研究
67