Hepatol Int:肝硬化的死亡率高于5种主要癌症的死亡率
2018-03-15 MedSci MedSci原创
肝硬化的死亡率高于5种主要癌症(肺癌、结直肠癌、胃癌、肝癌、乳腺癌)的死亡率
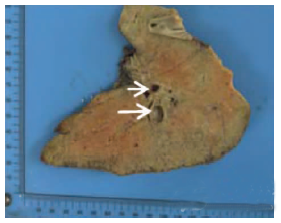
众所周知,肝硬化患者的生存率较低,肝硬化与其他致命疾病的关系的评估将有助于设计适当的健康干预措施。近日,发表在Hepatol Int上的一篇文章表明,肝硬化的死亡率高于5种主要癌症(肺癌、结直肠癌、胃癌、肝癌、乳腺癌)的死亡率。
此研究使用2002年至2010年,国家健康保险服务国家样本组(NHIS-NSC)的数据。研究共纳入韩国46,605,433人的1025340个有代表性的样本数据。
在8年之间,800/2609的肝硬化患者发生死亡,1316/4852的癌症患者,发生死亡。将肝硬化和五种主要癌症的死亡率进行评估时,肝硬化患者的相对死亡率更高[在对年龄、性别、居住地、保险类型、保费水平、并发症进行调整后,危险比为1.47 (95% CI 1.28-1.67)]。采用敏感性分析,排除即有肝硬化又存在5种主要癌症之一的患者,研究结果依然表明肝硬化的死亡率高于5种主要癌症的死亡率[危险比:1.27 (95% CI 1.10-1.47)]。此外,当研究将肝硬化患者局限于失代偿性肝硬化患者时,失代偿性肝硬化的相对死亡率甚至更高于五种癌症的死亡率[危险比1.82 (95%CI 1.51-2.20)]。
原始出处
Chung W; Jo C; Chung WJ; et al. Liver cirrhosis and cancer: comparison of mortality. Hepatol Int, 2018, 2018 Mar 1. doi: 10.1007/s12072-018-9850-5.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#EPA#
27
学习一下谢谢
58
学习
53