ATSIC 2016:新的结核皮肤试验C-Tb优于PPD试验
2016-05-18 Seven L 译 MedSci原创
美国胸学会2016国际会议称,一种新的潜伏结核皮肤测试不仅安全易使用,并解决了当前测试对接种BCG疫苗后出现假阳性的问题。基于抗原ESAT-6和CFP10,丹麦Statens Serum Intitut开发的新测试C-Tb。Statens Serum Institut的Morten Ruhwald博士说:“它结合了PPD结核菌素皮肤试验的优点,以及干扰素γ释放试验的高度特异性。”研究人员给出的数据
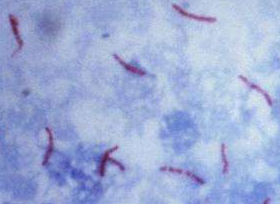
美国胸学会2016国际会议称,一种新的针对潜伏性结核的皮肤测试不仅安全易使用,并解决了当前测试对接种BCG疫苗后出现假阳性的问题。
基于抗原ESAT-6和CFP10,丹麦Statens Serum Intitut开发的新测试C-Tb。Statens Serum Institut的Morten Ruhwald博士说:“它结合了PPD结核菌素皮肤试验的优点,以及干扰素γ释放试验的高度特异性。”
研究人员给出的数据来自两个完成的3期临床试验,TESEC-05和TESEC-06。TESEC-05试验包含来自南非开普敦的1,090名结核病症状和100名对照参与者;TESEC-06试验包含西班牙加泰罗尼亚、加利西亚和巴斯克的13个临床试验地点的979名参与者,拥有结核杆菌感染的风险因素。
在这两项试验中,通过双盲方法对参与者的前臂进行C-Tb和结核菌素皮肤试验。2-3天后观察皮肤硬结情况。在皮肤试验之前对患者进行血液IGRA检测(Quantiferon, QFT-GIT)。
研究结果显示,与结核菌素皮肤试验相比,C-Tb的安全性是可以接受的。研究者对212名假定非暴露的西班牙对照组评估了检测的特异性,结果显示C-Tb与QFT-GIT的特异性具有可比性(均为97%, P = 1),并且不会受到BCG疫苗接种的影响。而目前的结核菌素皮肤试验对接种BCG疫苗和未接种人群的特异性分别为62%和95%(P < .001)。对于确诊结核的患者,C-Tb和QFT-GIT的敏感度也具有可比性(77% vs. 81%; P = .08)。此外,结核暴露与C-Tb测试阳性率的增加具有强烈的趋势。
原始出处:
Ruhwald M, et al. Diagnostic accuracy of the novel C-Tb skin test for latent M. tuberculosis infection: Results from two phase 3 clinical trials. Presented at the American Thoracic Society International Conference, May 13 to 18, 2016; San Francisco.
New TB skin test safe, easy to use.Healio.May 17, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ATS#
39
#皮肤试验#
40
不错哦继续关注
73
多了解
111
多学学?!
62
#结核#
34