J Am Soc Nephrol:卡格列净的蛋白尿早期变化可以预测肾脏和心血管结局(CREDENCE研究)
2021-08-23 MedSci原创 MedSci原创
卡格列净能够保护患者的肾脏,减少肾功能不全的发生风险,特别是减少因为肾脏衰竭所导致的终末期肾病或死亡的发生风险,还可保护患者的心脑血管系统,在这些方面都具有非常重要的意义。
备受瞩目的全球首个降糖药物的肾脏结局研究——CREDENCE研究的结果着实令人震撼!研究发现,SGLT2抑制剂卡格列净不仅能够显著降低肾脏事件风险,还可以降低心血管事件风险,同时具有良好的安全性。本文就介绍一下CREDENCE的研究内容。
背景:蛋白尿的早期变化和肾脏、心血管事件之间的联系主要是基于肾素-血管紧张素抑制系统。目前还不清楚这种关联是否与钠-葡萄糖协同转运蛋白(SGLT2)抑制有关。
方法:卡格列净和糖尿病肾病临床评估(CREDENCE)试验纳入了4401例2型糖尿病和CKD患者(尿白蛋白-肌酐比值[UACR]>300 mg/g)。试验后分析评估卡格列净对蛋白尿的影响以及早期蛋白尿如何变化(基线为26周)、与肾相关的结局(ESKD、血清肌酐翻番、或肾衰竭)、主要不良心血管事件(MACE)、心衰住院或心血管死亡(HHF/CV)。在CREDENCE试验中,共收集到3836名(87.2%)参与者蛋白尿和其他协变量早期变化的完整数据。
与安慰剂相比,卡格列净在26周降低了31%的UACR(95%置信区间[95% CI],27%~36%),并显著增加了UACR降低30%的可能性(优势比[OR],2.69;95%可信区间,2.35-3.07)。

图1 到第26周时,卡格列净降低了蛋白尿向肾病进展的可能(A组),增加蛋白尿消退的可能(B组)。
卡格列净可使蛋白尿发生几率降低≥30 %(OR,0.41;95%CI,0.3-0.48;P,0.001),并且增加了蛋白尿减少>30%的几率(OR,2.69;95%CI,2.35-3.07;P<0.001)
前26周UACR每降低30%,与原发性肾脏疾病的预后风险降低独立相关(风险比[HR],0.71;95% CI,0.67 - 0.76;P,0.001),主要心血管不良事件(HR,0.92;95% CI,0.88 -0.96;P,0.001)、心衰住院或心血管死亡(HR,0.86;95% CI,0.81-0.90;P 0.001)。
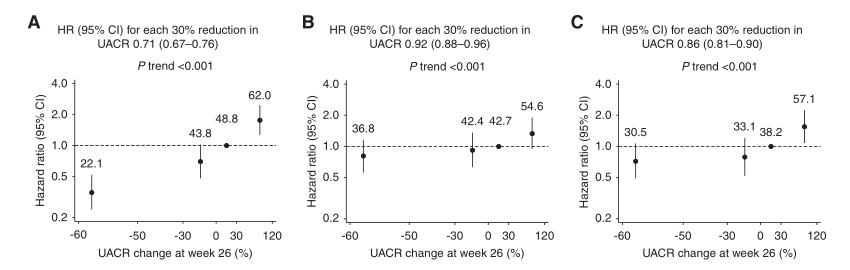
图2 第26周时蛋白尿的早期变化与(A)肾脏综合结局、(B) MACE和(C) HHF/CV死亡风险独立相关。
每个圆圈上面的数字代表UACR变化的发生率。
总的来说,在每个治疗组中,第26周的残余蛋白尿水平仍然是肾脏和心血管事件的一个强大的独立危险因素。
结论:在2型糖尿病和CKD患者中,使用卡格列净可使早期蛋白尿持续减少,这与长期肾脏和心血管预后独立相关。
在CREDENCE研究公布之日,《国际糖尿病》对该研究中国区PI——北京大学人民医院纪立农教授进行采访时,纪立农教授说道:卡格列净在有肾脏疾病高风险的2型糖尿病患者中有明确的肾脏保护作用,并且可能在不同人种和人群之间没有明显差异。CREDENCE研究结果的发布,将会更好地指导我们在有肾脏疾病高风险人群中使用这类药物,特别是卡格列净,能够保护患者的肾脏,减少肾功能不全的发生风险,特别是减少因为肾脏衰竭所导致的终末期肾病或死亡的发生风险,还可保护患者的心脑血管系统,在这些方面都具有非常重要的意义。
原文出处:
Oshima M, Neuen BL, Li J, et al. Early Change in Albuminuria with Canagliflozin Predicts Kidney and Cardiovascular Outcomes: A Post Hoc Analysis from the CREDENCE Trial. J Am Soc Nephrol. 2020. 31(12): 2925-2936.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#心血管结局#
44
#CRE#
39
阅读
54
又一个sglt2i的肾脏研究
49
保护糖尿病患者肾功能
51