Cell metab:运动能预防2型糖尿病?这事儿肠道菌说了算!
2019-12-01 佚名 中国生物技术网
在医学界,大多数观点认为2型糖尿病是可以预防的,只要改变饮食习惯和增加锻炼即可。但事情可能不像我们想象的那么简单。运动并不总能导致葡萄糖代谢下降。
临床研究发现,运动对于改善代谢的效果具有巨大的差异性,单纯运动并不能显着改善部分人的代谢机能,甚至有少部分人的情况会因运动而变得更差。这种通称为“运动抵抗”的现象,其病理机制至今尚未查清,极大地限制了运动疗法的推广和应用。
近日,发表在《Cell Metabolism》上的一篇研究表明,肠道微生物组(肠道菌群)及其代谢产物对于运动治疗在改善代谢的效果方面有着重大影响,并揭示了部分糖尿病前期患者在接受运动治疗后,代谢改善效果不佳的原因。
这项由香港大学李嘉诚医学院(港大医学院)徐爱民教授领导的研究团队发现,肠道菌群的组成可以作为判断糖尿病前期患者运动效果的一个指标。这项针对运动治疗,并结合了随机对照的人体实验,以及小鼠模型的研究,首次为肠道菌群对运动治疗在改善身体代谢机能的情况提供了直接的因果证据。该团队还包括来自港大医学院内科学系、港大运动中心、德国汉斯诺尔研究所以及广东药科大学的研究人员。
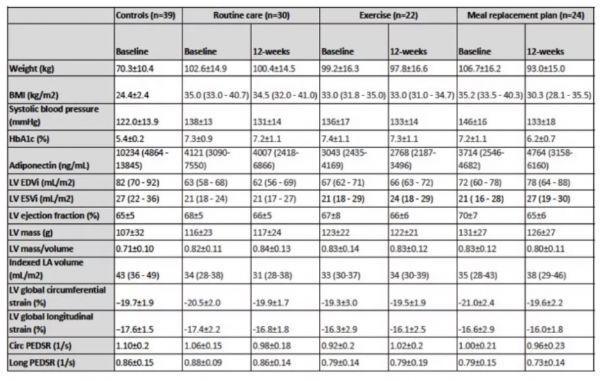
在这项研究中,研究团队从本地社区中招募了771名志愿者,经过筛选后,对其中39名超重且糖耐量受损的参与者(糖尿病前期)展开了为期12周的高强度运动介入治疗。
经过12周治疗后,虽然所有参与者在没有任何药物和膳食调节的前提下,体重和体脂均有大致相同程度的下降,然而糖代谢指标的改善程度却表现出巨大差异。其中70%的参与者血糖水平显着下降(运动有效者),其余30%的参与者血糖水平则几乎没有变化(运动无效者)。
通过结合宏基因组学及代谢组学的分析,研究团队发现,“运动有效者”和“运动无效者”的肠道菌群变化存在显着差异。具体而言,经过高强度运动治疗后,“运动有效者”的肠道菌群在合成短链脂肪酸、分解支链氨基酸等功能上均有显着增强;而“运动无效者”的肠道菌群则会合成大量不利于糖代谢的产物,如支链氨基酸、芳香族氨基酸等。
随后,研究人员将“运动有效者”的肠道菌群移植到肥胖小鼠中进行测试,发现其胰岛素敏感性显着提升;而如果将“运动无效者”的肠道菌群移植至小鼠,则无法改善其血糖水平。另一方面,如果向移植了“运动抵抗”菌群的小鼠提供额外的短链脂肪酸,动物糖代谢紊乱的状态会得到有效的逆转。
研究团队还发现,运动治疗前通过对不同参与者的肠道菌群特征进行评估,可以准确预测运动治疗对糖尿病前期病人的效果。针对另一批30名的糖尿病前期患者,研究人员通过人工智能技术,利用肠道菌群及其代谢产物构建出的预测模型,可以准确预测运动对他们糖代谢改善的效果。肠道菌群及其代谢产物有望成为评估和预测运动干预疗效的生物标志物。
目前运动介入治疗已被广泛应用于预防多种疾病上,肠道菌群及其代谢物或可成为运动介入治疗效果的监测指标。通过监测肠道菌群的变化,临床医生和运动专家将能更有效地评估个体在运动治疗中获益的程度,并可以通过调节肠道菌群来帮助那些运动治疗效果不佳的患者,使他们可以从运动治疗中获得更大益处。这项研究为制定个性化糖尿病早期预防措施提供了新思路。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cell#
33
#Meta#
35
#MET#
36
#CEL#
38
#肠道菌#
39
谢谢MedSci提供最新的资讯
36
学习了,谢谢分享
66
学习了,谢谢分享
75
学习了,谢谢分享
64
学习了,谢谢分享
72