肥胖相关性高血压管理中国专家共识:以下九种情况可能为继发性肥胖
2016-12-20 许菁 中国循环杂志
胖与高血压常常合并存在,不仅增加血压控制难度,还促进多重心血管代谢危险因素聚集,显著增加心脑血管疾病风险。中华医学会心血管病学分会高血压学组于今年3月发布的《肥胖相关性高血压管理的中国专家共识》提出了肥胖相关性高血压的概念并制定了诊断流程。《共识》建议伴有下述临床症状与体征的肥胖相关性高血压患者进行肥胖继发性病因临床评估及确诊检查: (1)向心性肥胖、水牛背、锁骨上脂肪垫;满月脸、多血质;皮肤菲薄
胖与高血压常常合并存在,不仅增加血压控制难度,还促进多重心血管代谢危险因素聚集,显著增加心脑血管疾病风险。中华医学会心血管病学分会高血压学组于今年3月发布的《肥胖相关性高血压管理的中国专家共识》提出了肥胖相关性高血压的概念并制定了诊断流程。
《共识》建议伴有下述临床症状与体征的肥胖相关性高血压患者进行肥胖继发性病因临床评估及确诊检查: 
(1)向心性肥胖、水牛背、锁骨上脂肪垫;满月脸、多血质;皮肤菲薄、瘀斑、宽大紫纹、 肌肉萎缩;
(2)高血压、低血钾、碱中毒;
(3)糖耐量减退或糖尿病;
(4)骨质疏松、或有病理性骨折、泌 尿系结石;
(5)性功能减退,男性阳痿,女性月经紊乱、多毛、不育等;
(6)儿童生长、发育迟缓;
(7)神经、精神症状;
(8)怕冷、水肿;
(9)易感染、机体抵抗力下降。
共识提出,肥胖相关性高血压诊断的确立有两个要点:一是肥胖和高血压的诊断切点;二是排除其他继发性高血压。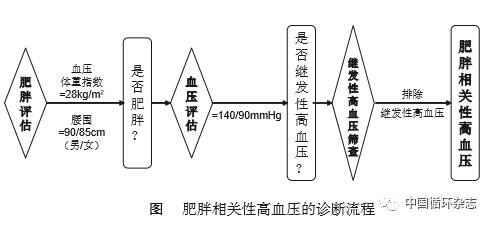
本《共识》仍然沿 用 140/90 mmHg 这一诊断切点。但特别强调,对于肥胖人群,要选择合适的袖带准确测量血压尤为重要。
本《共识》强调,肥胖相关性高血压的干预应当兼顾血压控制、体重控制和改善代谢紊乱三个方面。着重阐述关于体重和血压的管理,治疗策略上应根据病情贯彻综合干预和个体化治疗原则,特别要注意生活方式的改善,在药物选择上应降压和改善代谢紊乱并重。
在体重控制方面,对于生活方式干预无效的肥胖相关性高血压患者,《共识》建议可考虑使用减肥药物。如果生活方式干预+药物治疗均不理想的难治性肥胖相关性高血压患者,代谢手术治疗是获得长期减肥效果和改善心血管预后的重要手段。
在药物治疗方面,《共识》建议 RAS 抑制剂作为肥胖相关性高血压的首选治疗用药,钙拮抗剂可作为肥胖相关性高血压的联合治疗用药, 小剂量利尿剂也可联合使用。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#专家共识#
31
#继发性#
28
#相关性#
26
#中国专家共识#
31
#继发#
33
#高血压管理#
23
#血压管理#
34
好共识,学习下
52