BMJ:社区获得性肺炎(CAP)患者入院时血糖水平高,预示死亡风险增加
2012-06-17 刘伟杰 编译 中国医学论坛报
Fig 1Cumulative incidence of death (%) within 90 days in participants with community acquired pneumonia stratified by serum glucose levels on admission overall (n=6016) (top) and without diabetes (n=5
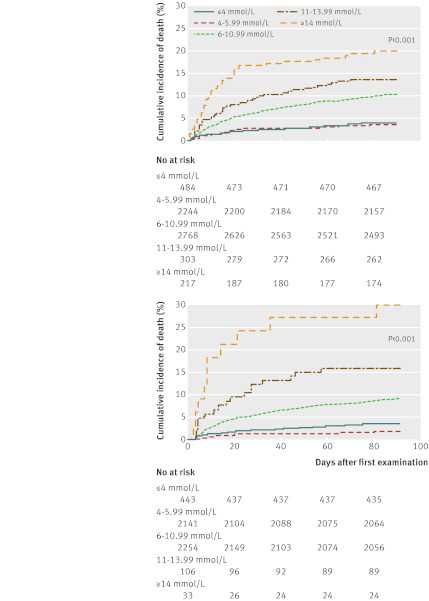
Fig 1 Cumulative incidence of death (%) within 90 days in participants with community acquired pneumonia stratified by serum glucose levels on admission overall (n=6016) (top) and without diabetes (n=5141) (bottom). The 875 participants with missing data for serum glucose levels on admission were not included in these calculations for patients at risk
Cumulative incidence of death (%) within 90 days in participants with community acquired pneumonia stratified by serum glucose levels on admission overall (n=6016) (top) and without diabetes (n=5141) (bottom). The 875 participants with missing data for serum glucose levels on admission were not included in these calculations for patients at risk
一项多国联合研究显示,既往无糖尿病,但入院时有急性高血糖症的社区获得性肺炎(CAP)患者面临更高的死亡风险。论文5月29日在线发表于《英国医学杂志》(BMJ)。
研究者共收集了2003年~2009年间来自德国、瑞士和奥地利的6891例CAP患者数据,在校正性别、年龄、当前吸烟状况、CAP严重程度及各种共病因素后,评估了入院时不同血糖水平与患者28、90和180天死亡率的相关性。
结果为,既往无糖尿病但入院时血糖水平升高,是CAP患者28天和90天内死亡的预测因子。与入院时血糖水平正常者相比,存在轻度急性高血糖症者(血糖水平6~10.99 mmol/L)90天内死亡风险显著增加[危险比(HR)=1.56,P<0.001],当患者入院时血糖水平≥14 mmol/L时,90天内死亡风险也随之进一步升高(HR=2.37,P<0.001)。此外,与无糖尿病患者相比,既往患糖尿病者总体死亡率显著升高(HR=2.47,P<0.001)。这一结果不受入院时患者血糖水平的影响(P=0.18)。
原始文献:
Lepper PM, Ott S, Nüesch E, von Eynatten M, Schumann C, Pletz MW, Mealing NM, Welte T, Bauer TT, Suttorp N, Jüni P, Bals R, Rohde G; on behalf of the German Community Acquired Pneumonia Competence Network (CAPNETZ).Serum glucose levels for predicting death in patients admitted to hospital for community acquired pneumonia: prospective cohort study. BMJ. 2012 May 28;344:e3397. doi: 10.1136/bmj.e3397.
免费全文下载:PDF (558K)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CAP#
49
#获得性#
51
#BMJ#
43
#血糖水平#
51
#死亡风险#
41
#社区#
50