Hepatology:瞬时弹性成像可分辨胆道闭锁(BA)患儿和在肝门肠吻合术后,LSM检测可预测BA患儿的预后
2018-03-05 MedSci MedSci原创
LSM检测,可能能够在胆汁阻塞性幼儿中,分辨出BA患儿。肝门肠吻合术后,LSM检测可能能够预测BA患儿的并发症和需要进行肝移植的患儿
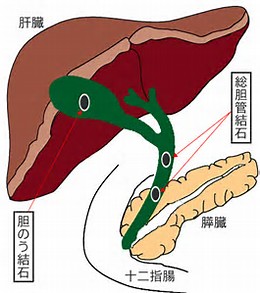
研究背景:本研究旨在调查瞬时弹性成像在胆汁阻塞性婴儿胆道闭锁(BA)诊断中的应用和预测胆道闭锁(BA)疾病预后的价值。
研究方法:本研究共纳入48例胆汁郁积的婴幼儿(年龄:9-87天),直接胆红素> 1 mg/dL。胆汁淤积的过程中,采用瞬时弹性成像进行肝硬度检测(LSM),其中15例患儿被诊断为胆道闭锁。36例患儿进行肝穿,评估肝脏组织学;采用METAVIR评分系统,判定肝脏肝纤维化分期。
研究结果:相比非胆道闭锁(BA)的婴幼儿,胆道闭锁(BA)的婴幼儿LSM值和METAVIR评分显著增高。受试者工作特征曲线分析表明,在胆汁阻塞性幼儿中,LSM >7.7 kPa可预测患儿发生胆道闭锁(BA)(敏感性= 80%,特异度= 97%,曲线下面积= 85.3%,P = 0.0001)。LSM >7.7 kPa的胆汁阻塞性幼儿,很可能被诊断为BA (比值比 = 128, P < 0.001)。肝门肠吻合术后,LSM的及早期检测与肝门肠吻合术6个月后,血小板减少,脾肿大,食管静脉曲张有关。其中五名患者正在等待或已经接受肝移植,相比其他的BA患儿,这5名患儿在肝门肠吻合术1周后,LSM测量值显著增高(26.0 vs. 10.8 kPa, P = 0.006)。Cox比例分析表明,在肝门肠吻合术1周后,相比其他的BA患儿,等待肝移植的BA患儿,LSM > 16 kPa的比例更高(风险比 = 10.16, P = 0.04).。
研究结论:LSM检测,可能能够在胆汁阻塞性幼儿中,分辨出BA患儿。肝门肠吻合术后,LSM检测可能能够预测BA患儿的并发症和需要进行肝移植的患儿。
原始出处
Wu JF, Lee CS, Lin WH, et al. Transient elastography is useful in diagnosing biliary atresia and predicting prognosis after hepatoportoenterostomy. Hepatology, 2018, Feb 27. doi: 10.1002/hep.29856.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#瞬时弹性成像#
25
#弹性成像#
23
#吻合术#
29
#EPA#
34
#胆道闭锁#
32
学习.
42
不错的文章值得拥有
47
谢谢分享学习
51
不错的文章.值得推荐
36
^_^^_^^_^
48