JNCI Cancer Spectrum:姐妹们太阳晒起来!补充钙+维生素D可降低乳腺导管内原位癌风险!
2021-09-08 MedSci原创 MedSci原创
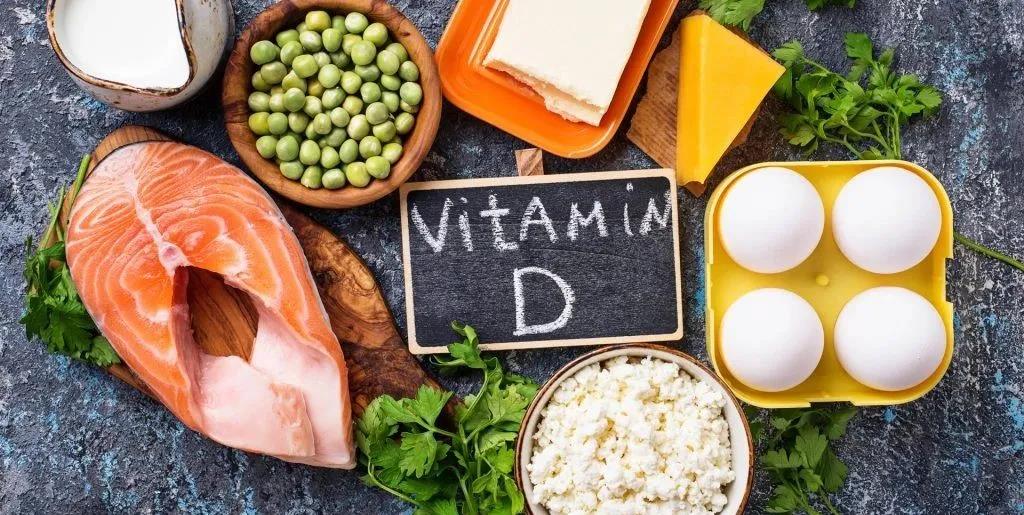
超3万绝经后女性随访数据显示,,钙+维生素D的补充可以降低乳腺DCIS的风险,提高CaD补充或能通过在疾病自然史的相对早期阶段发挥作用,最终降低乳腺癌风险。
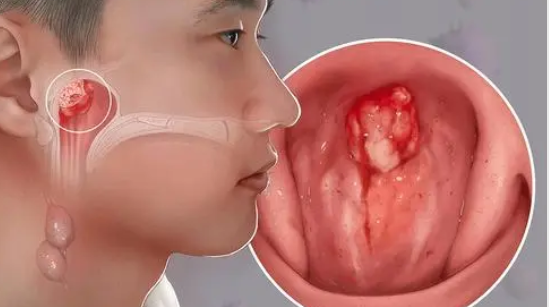
导管原位癌( Ductal Carcinoma In Situ,DCIS)是以局限在乳腺基底膜内为特征的上皮细胞增殖,它被认为是乳腺浸润性导管癌的癌前病变,约15%~50%的病例在10年或以后可能发展为浸润癌。DCIS确诊后,乳腺癌发生和死亡风险增加将持续至少20年。流行病学研究表明,DCIS与浸润性乳腺癌,其中实验证据表明,钙和维生素D对乳腺癌有潜在的保护作用,其血清浓度水平很可能与乳腺癌风险呈负相关。

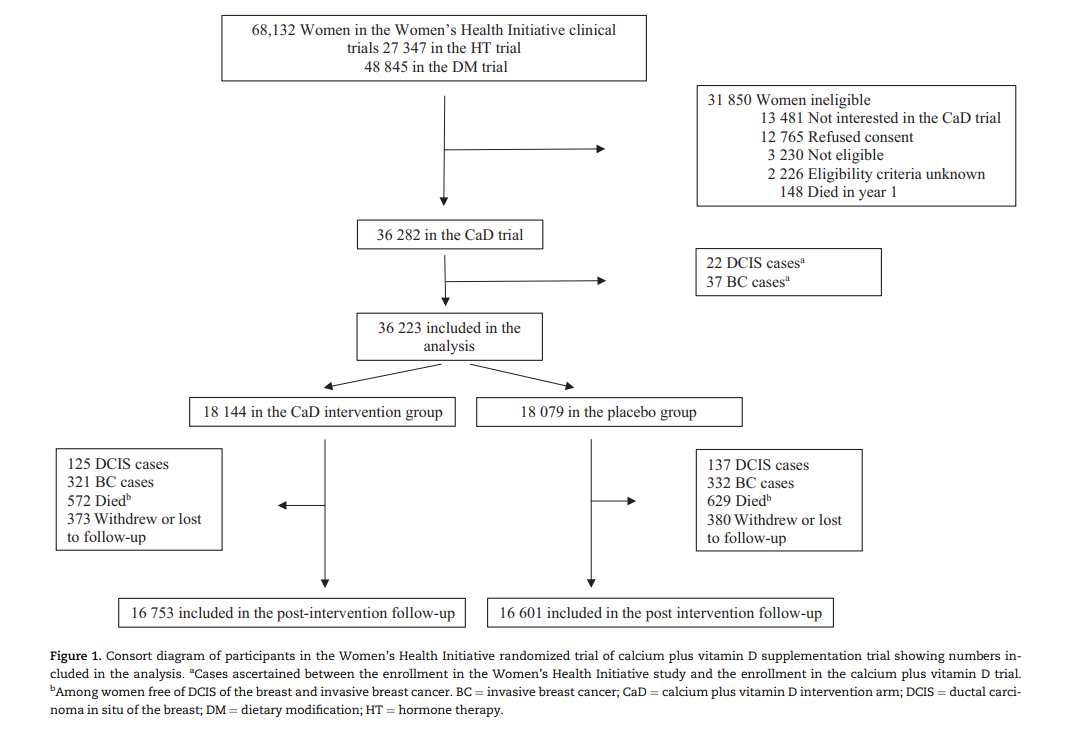
本研究随访了妇女健康倡议(WHI)的钙加维生素D的随机对照实验,这项实验囊括36282名无癌症的绝经后(50-79岁)妇女,她们被随机分配到干预组(每天1000mg碳酸钙+400IU维生素D3)或安慰剂组中。本研究的主要目的是评估在整个随访期间(干预期及干预后),钙和维生素D补充剂与乳腺导管原位癌风险的关系,采用Kaplan-Meier法估算DCIS的发生率,log-rank检验P值比较生存曲线。
总的来说,在整个随访期间确诊了595例DCIS(风险中位时间为18.7年;四分位区间10.7-20.9年),共有262例病例发生在干预阶段(风险中位数时间为7.1年),333例病例发生在干预后阶段(风险中位数时间为13.8年)。

Kaplan-Meier估计的DCIS在整个随访期间的干预状态累积危害
伴随的IRs显示,干预组在每个时间点的DCIS风险均低于对照组(干预IR/1000人-年 5、10、15、20、大于20年¼1.07、1.08、0.86、0.84和0.51;对照组IR/1000人-年5、10、15、20,大于20年¼分别为1.15、1.19、1.40、1.02、0.59)。分配给干预手臂女性DCIS风险降低了18.0% (HR¼0.82,95% CI¼0.70到0.96)。类似的结果分析时调整的乳房x光检查和临床乳腺检查频率(HR¼0.80,95% CI¼0.68到0.95),在排除纳入随访时间少于1年的参与者(HR¼0.81,95% CI¼0.68 - 0.97),或在排除既往乳腺活检的女性后(HR¼0.72,95% CI¼0.59 - 0.86)。检查依从性低于80.0%或50.0%的女性对结果没有影响(HR¼0.81 [95% CI¼0.68 - 0.96]和HR¼0.82 [95% CI¼0.69 - 0.96])。
Fine-Gray模型的结果也显示,与对照组相比,干预组DCIS的相对发生率降低(亚分布HR¼0.82,95% CI¼0.70至0.97)。如先前报道的,在干预期间,补充CaD与DCIS风险改变无关(HR¼0.91,95% CI¼0.71 - 1.15)。相比之下,干预后风险显著降低(HR¼0.76,95% CI¼0.61 - 0.94)。
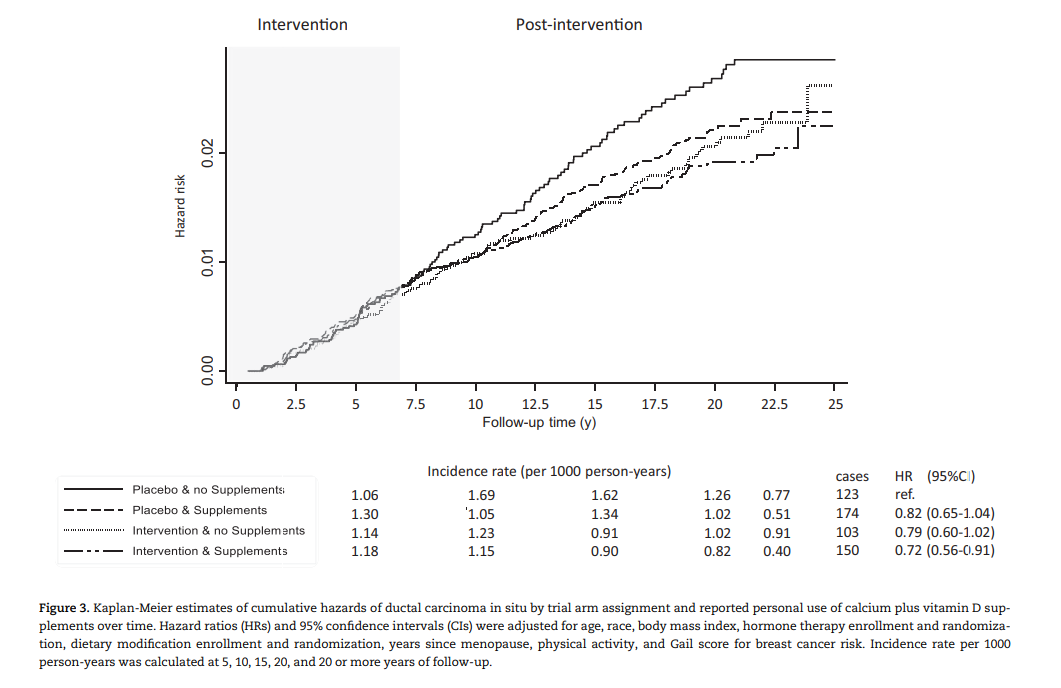
根据干预状态和个人补充钙和维生素D的使用定义的组的间隔时间IRs、累积发病率和危险比
与安慰剂组在整个试验期间没有服用补充剂的女性相比,干预组使用补充剂的女性在干预结束后有更低的IRs,并降低了DCIS风险(HR¼0.72,95% CI¼0.56到0.91)。而在其他两组,IRs和HR无统计学意义。
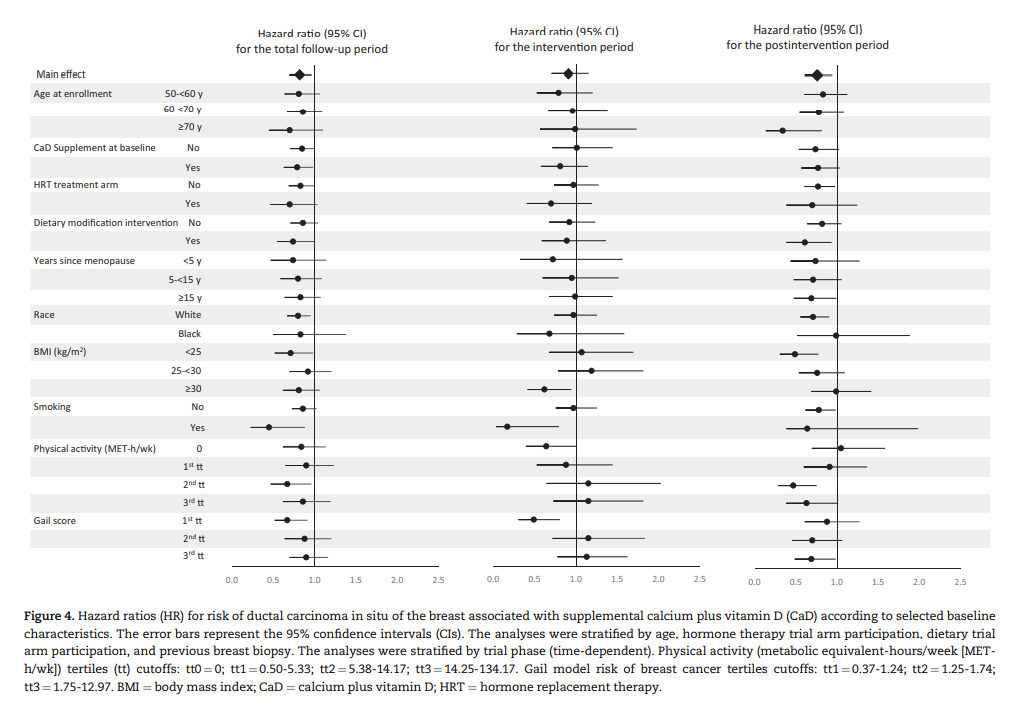
在整个随访期间,在受DCIS各种潜在危险因素影响的子组中,尽管在统计学上大多并不显著,但仍有一些降低风险的迹象。仅限于干预阶段的分析显示,大多数关联接近于零,尽管有一些证据表明BMI (Pinteraction¼.046)、娱乐体育活动(Pinteraction¼.047)、吸烟(Pinteraction¼.03)和Gail模型评分(Pinteraction¼.001)的亚组之间存在异质性。
随访7年后,两组中发生浸润性乳腺癌和DCIS的风险相似。随后的分析包括干预期结束5年后发生的结果,浸润性乳腺癌发生风险的结果类似,但DCIS风险显著降低。目前的分析表明,在WHI试验的整个随访期间(包括明显延长的大约13.8年的干预后),补充CaD与乳腺癌DCIS风险的相关性。
在对数据的二次分析中,我们发现干预与降低乳房DCIS的风险有关。在排除随访时间少于1年或在试验开始前进行乳房活检的患者后,这些结果仍具有统计学意义。
总之,这项研究的结果表明,钙+维生素D的补充可以降低乳腺DCIS的风险。考虑到DCIS是乳腺癌的癌前病变,这些发现提高了CaD补充可能通过在疾病自然史的相对早期阶段发挥作用,最终降低乳腺癌风险的可能性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#癌风险#
0
#PE#
37
#原位癌#
43
#NCI#
41
DCIS与CaD关系密切~
0
#乳腺癌#与#VitD#当然有关了
114