胡锡琪:药物性肝损伤组织病理学评分
2012-06-17 庞琳娜 复旦大学上海医学院
由于肝脏是药物代谢的重要脏器,因此随着各种新药的不断涌现,药物性肝损害(drug-induced liverinjury,DILI)逐年增多,已知超过600多种药物可引起DILI。由于肝穿刺是一种创伤性的诊断措施,标本来之不易,所以临床对病理诊断的期望值过高,被誉为“金标准”,然而DILI的病理学变化均为非特
由于肝脏是药物代谢的重要脏器,因此随着各种新药的不断涌现,药物性肝损害(drug-induced liverinjury,DILI)逐年增多,已知超过600多种药物可引起DILI。由于肝穿刺是一种创伤性的诊断措施,标本来之不易,所以临床对病理诊断的期望值过高,被誉为“金标准”,然而DILI的病理学变化均为非特异性,可见“金标准”在DILI面前显得含金量不足。
受慢性肝炎计分评估(Scoring of CH)、非酒精性脂肪性肝病活动度评分(Nonalcoholic fatty liver discase active score,NAS)和国际自身免疫性肝炎组评分(International AIH Group scoring system)的启示,复旦大学上海医学院病理学系胡锡琪教授,自2000年起注意收集DILI的种种病理变化,并逐一加以评分,形成DILl评分系统DILl-PSS(DILI-pathological scroring system),该标准2010年形成第一稿,2012在初稿的基础上进行改进形成修改稿。
药物性肝炎的主要病理学变化包括:
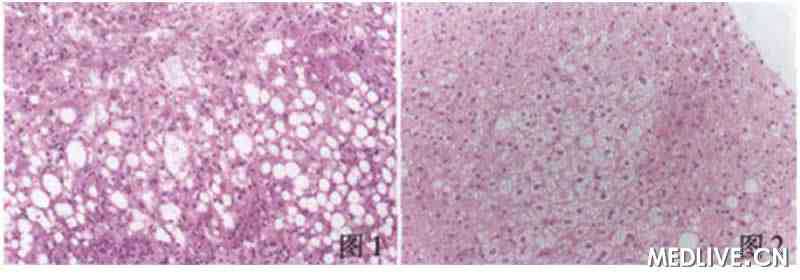
1.肝细胞脂肪变性(DILI-PSS3):可以大泡性脂肪变性(DILI-PSS1,图1)和(或)小泡性脂肪变性(DILI-PSS2,图2)。小泡性脂肪变性意义更大,具有相对特异性。小泡性脂肪变性的肝细胞膜下见无数细小张力型空泡,整个肝细胞形如泡沫状,故称之泡沫细胞。婴幼儿因水杨酸制剂引起的Reye综合征和四环素引起的DILI可导致几乎所有肝细胞呈泡沫状。

图1 大泡性细胞变性;图2 小泡性细胞变性
2.肝细胞性胆汁淤积(DILI-PSSl):肝细胞胞质内显现棕黄色胆汁颗粒,伴毛细胞胆管扩张,胆栓形成,呈现花环样图像(图3),病变以小叶中央区为明显。

图3 肝细胞胆汁淤积;图4 肝细胞凋亡
3.肝细胞凋亡(DILI-PSS1):在肝索和血窦内可见单个圆形匀质的嗜伊红小体(图4),数量多,分布广,十分引入注目。肝细胞坏死,包括点灶性坏死,碎屑样坏死或界面肝炎,亚大块肝坏死,和大块肝坏死,这些病变与病毒性肝炎相似,不予评分,但必须记录在案,必要时作Ishak的HAI评估。
4.嗜伊红白细胞浸润(DILI-PSS2):坏死区和门管区嗜伊红白细胞浸润,有时血窦内亦可见(图5)。在除外寄生虫和嗜酸性肉芽肿后,对DILI诊断具相对特异性。

图5 嗜伊红白细胞浸润;图6 上皮内肉芽肿
5.上皮内肉芽肿:由于药物对肝脏是一种异物,其可被巨噬细胞(枯否细胞)吞噬,形成由类上皮细胞,多核巨噬细胞和淋巴细胞组成的肉芽肿(图6),肉芽肿中心不含凝固性坏死。在本文收集的并最后得到临床确诊的DILI肝穿标本中,肉芽肿的检出率仅为4%,故对肉芽肿评分调整为附加分1分。

图7 铁沉着
6.铁沉着:肝细胞坏死区,尤其是桥样坏死网状支架塌陷区铁沉着(图7)。是含铁药物引起DILI的佐证。因其检出需作特殊染色,而一般病理科不做这种特殊染色,对其评分也调整为附加分1分。
综上所述,DILI-PSS包括:肝细胞脂肪变性3(大泡性1,小泡性2),肝细胞性胆汁淤积1,凋亡小体1,嗜伊红白细胞浸润2,总计7分,另有上皮性肉芽肿附加1,坏死区铁沉着附加1。根据DILI-PSS得分高低,受DILI临床因果关系5阶法评估的启示提出(如下表)。
表:DILl病理因果关系5阶法评估
| DILI-PSS | DILI-Pathol 5-PS |
| 8~9 | 明确(Definit) |
| 7 | 极可能(Highly likely) |
| 5~6 | 很可能(Probable) |
| 3~4 | 可能(Possible) |
| 1~2 | 不可能(Unlikely) |
建议DILI病理诊断报告书写格式:
1.组织病理学形态描述,DILI-PSS;
2.病理诊断:肝炎+DILI-Pathol-5PS。
参考文献:中华肝脏病杂志, 2012;20(3):176-7.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#组织病理学#
31
#肝损伤#
31
#损伤#
31
#病理学#
37
#药物性#
34