药物性肝损伤:筛查基因或可预知危险
2011-01-10 MedSci原创 MedSci原创
英国学者唐纳森等的研究证实,人类白细胞(HLA)-DRB1*15等位基因是发生阿莫西林/克拉维酸 DILI的危险因素。此外,研究者还首次发现,HLA-DRB1*07的表达对阿莫西林/克拉维酸DILI的发生具有显著的保护作用。该研究发表在12月的《肝脏病学杂志》(J Hepatol 2010,53:1049)上。 在该研究中,研究组患者61例(均发生阿莫西林/克拉维酸DILI),对照组包括
英国学者唐纳森等的研究证实,人类白细胞(HLA)-DRB1*15等位基因是发生阿莫西林/克拉维酸 DILI的危险因素。此外,研究者还首次发现,HLA-DRB1*07的表达对阿莫西林/克拉维酸DILI的发生具有显著的保护作用。该研究发表在12月的《肝脏病学杂志》(J Hepatol 2010,53:1049)上。 在该研究中,研究组患者61例(均发生阿莫西林/克拉维酸DILI),对照组包括人群对照组(191名未接受过阿莫西林/克拉维酸的白人)和治疗对照组(40名来自医院或社区医院、接受过阿莫西林/克拉维酸处方、但未发生阿莫西林/克拉维酸DILI的白人)。比较3组研究对象在HLA等位基因和基因型方面的差异。 图 HLA-DRB位点相关基因可能与患者是否发生阿莫西林/克拉维酸相关DILI有关 阿莫西林/克拉维酸虽然安全性较好,但也可引起药物相关性肝损伤(DILI)。 该研究有2个重要发现,第一,与治疗对照(33%)和人群对照组(30%)相比,HLA-DRB1*15在发生阿莫西林/克拉维酸DILI的患者中较多[53%,与治疗对照相比,比值比(OR)为2.29;与人群对照相比,OR=2.59,P=0.002]。第二,DILI组中的HLA- DRB1*07较治疗对照组和人群对照组少见,分别为9.8%、35%(OR=0.18,P=0.0011)和29% (OR=0.266,P=0.0019)。[3140101] (舒扬) 链接 2009年,英国学者在发生氟氯西林DILI患者和对照者中,采用866399个标记物进行高通量全基因组关联研究(GWAS,该技术是一种用来寻找基因变异与表型之间关系的遗传学技术,近年在医学遗传学领域中发展迅速),首次确定了HLA-B*5701等位基因是发生氟氯西林DILI的危险因素,有HLA-B*5701等位基因者的氟氯西林DILI危险显著升高(Nat Genet 2009,41:816)。该项研究开创了探索DILI发生机制研究的新纪元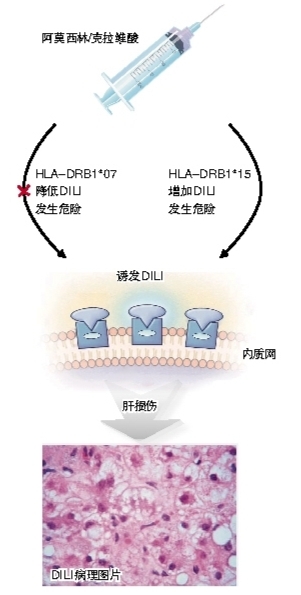
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肝损伤#
33
#损伤#
30
#药物性#
20