Mol Ther Nucleic Acids:HOTAIR或是晚期结肠直肠癌新的治疗靶标
2017-09-29 MedSci MedSci原创
晚期结肠直肠癌(CRC)治疗失败的一个主要原因是基于氟化嘧啶(FU)化疗的耐药性的出现。长链非编码RNA HOTAIR已被认为是多种癌症的致癌基因。然而,HOTAIR在化学耐药性中的确切功能机制尚不清楚。在本研究中,研究人员调查了HOTAIR在CRC的5FU耐药性中的生物学和临床作用。结果显示,HOTAIR通过EZH2靶向miR-218-2启动子调节轴负责调控CRC中的miR-218表达。敲低HO
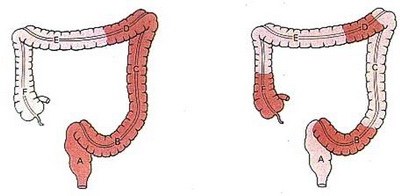
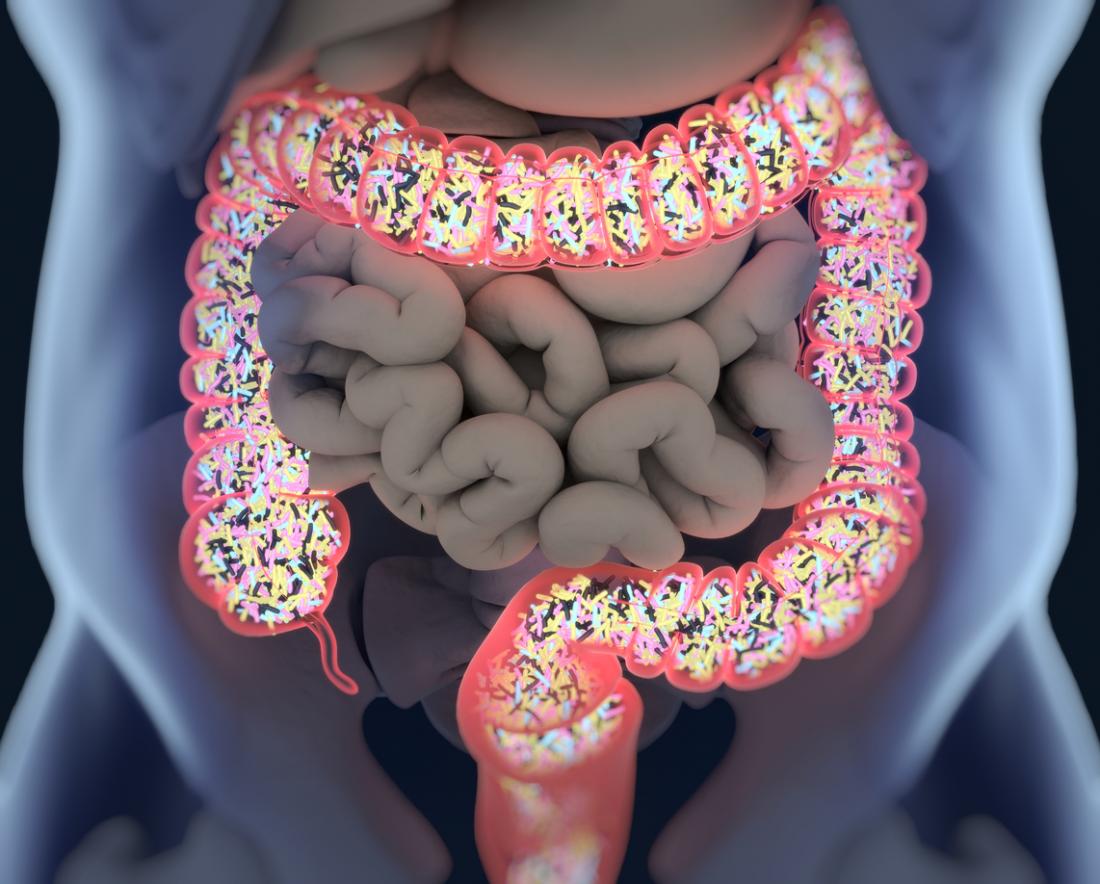
晚期结肠直肠癌(CRC)治疗失败的一个主要原因是基于氟化嘧啶(FU)化疗的耐药性的出现。长链非编码RNA HOTAIR已被认为是多种癌症的致癌基因。然而,HOTAIR在化学耐药性中的确切功能机制尚不清楚。 在本研究中,研究人员调查了HOTAIR在CRC的5FU耐药性中的生物学和临床作用。结果显示,HOTAIR通过EZH2靶向miR-218-2启动子调节轴负责调控CRC中的miR-218表达。敲低HOTAIR可通过促进miR-218的表达来显著抑制细胞活力并诱导G1期阻滞。研究显示VOPP1是miR-218的功能靶标,HOTAIR通过抑制miR-218表达使下游信号传导通路NF-κB失活。 此外,敲除HOTAIR可通过促进miR-218的表达和NF-κB信号传导失活部分逆转5FU耐药性。进一步,HOTAIR通过促进胸苷酸合酶表达来限制5FU诱导的对CRC细胞的细胞毒性。更重要的是,HOTAIR高表达与5FU治疗反应不良有关。 总之,该研究结果表明HOTAIR通过抑制miR-218的表达和激活CRC中的NF-κB信号来促进5FU耐药性。因此,HOTAIR可以作为治疗CRC患者的新的治
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#治疗靶标#
32
#CID#
30
#acid#
31
#HOTAIR#
38
#靶标#
28
#结肠直肠癌#
24
学习
55
学习了.涨知识
53