艾伯维关节炎新药upadacitinib抵达3期终点 效果优于Humira
2018-04-10 佚名 药明康德
艾伯维(AbbVie)公司今日宣布,其3期临床试验SELECT-COMPARE取得积极的顶线结果。结果显示,upadacitinib(每日一次15 mg)在给药12 周后,与安慰剂相比,对类风湿性关节炎患者达到了ACR20的主要终点和临床缓解。与adalimumab (阿达木单抗,Humira®,每隔一周40 mg)或安慰剂相比,达到所有次要终点。
艾伯维(AbbVie)公司今日宣布,其3期临床试验SELECT-COMPARE取得积极的顶线结果。结果显示,upadacitinib(每日一次15 mg)在给药12 周后,与安慰剂相比,对类风湿性关节炎患者达到了ACR20的主要终点和临床缓解。与adalimumab (阿达木单抗,Humira®,每隔一周40 mg)或安慰剂相比,达到所有次要终点。

类风湿性关节炎影响了全球约2770万人,是一种慢性和衰弱性疾病。在发达国家中,成年人发病率为0.5%至1%之间,中年发病率最高,女性发病率是男性的2.5倍。在2013年,有38000人死于该病。虽然该疾病的病因尚不清楚,但可能受遗传和环境因素的综合影响,导致身体的免疫系统攻击关节,引发疾病。尽管有多种可用的治疗方法,但许多类风湿性关节炎患者仍未达到临床缓解或低疾病活动的目标。
艾伯维带来的upadacitinib(曾用名ABT-494)是一种口服Janus激酶亚型1(JAK1)选择性抑制剂。JAKs属于细胞质酪氨酸激酶家族,其功能是转导细胞因子(如干扰素)介导的信号。共有四种JAK亚型,亚型之间有重叠的结合对象。这种激酶家族的抑制剂已经显示出治疗某些炎性和自身免疫性疾病(如类风湿性关节炎和克罗恩病)的功效。然而,第一代药物缺乏亚型选择性,导致药物的剂量依赖性副作用。Upadacitinib是第二代Janus激酶抑制剂,其对JAK1亚型具有高度选择性。Upadacitinib正在多个适应症中进行临床研究,如类风湿性关节炎、银屑病关节炎、克罗恩病、溃疡性结肠炎、特应性皮炎和巨细胞动脉炎。
此次进行的SELECT-COMPARE是一项3期多中心、随机、双盲研究,旨在评估upadacitinib与安慰剂和阿达木单抗相比,在稳定的甲氨喋呤背景下在中度至重度类风湿性关节炎成人患者中的疗效和安全性。患者接受甲氨喋呤背景治疗,随机按2:2:1接受upadacitinib、安慰剂或阿达木单抗治疗。第一阶段的主要终点包括与安慰剂相比治疗12周后达到ACR20*和临床缓解的受试者比例。次要终点包括与安慰剂相比修饰的总夏普得分(mTSS)改变,以及与阿达木单抗相比达到ACR50的受试者比例、低疾病活动度(LDA)、疼痛变化(VAS)和身体功能的改变。

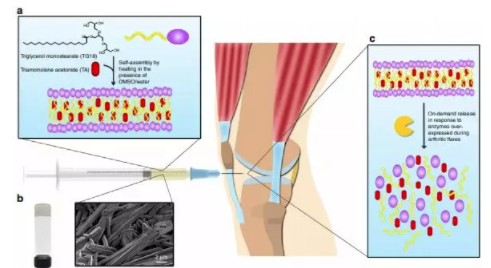
▲具体临床结果(图片来源:AbbVie官方网站)
结果显示,upadacitinib具有比安慰剂更好的ACR20疗效(71%对36%),且在一系列次要终点上疗效优于阿达木单抗(ACR50:45%对29%;ARC70:25%对13%;临床缓解率:29%对18%)。此外,upadacitinib的安全性与先前报道的结果一致,没有发现新的安全性信号。
艾伯维开发和首席科学官兼研究执行副总裁Michael Severino博士表示:“与安慰剂相比,这些结果显示出(upadacitinib)对症状和影像学进展的显著影响,以及与阿达木单抗相比,ACR反应和低疾病活动等重要措施的改善。我们对这些强有力的结果感到兴奋,这些结果增加了大量证据,支持upadacitinib成为类风湿性关节炎患者的重要治疗选择。”
艾伯维表示,将于2018年下半年为upadacitinib提交全球监管意见书,作为针对类风湿性关节炎的治疗药物。我们期待着它的好消息,希望尽快为类风湿性关节炎患者带来福音!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













***
80
#miR#
32
#CIT#
35
#ADA#
27
#关节炎#
35
#艾伯维#
34
#Humira#
0