本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2018-04-04 胡鉴瑜 欧云生 杜兴 中国矫形外科杂志
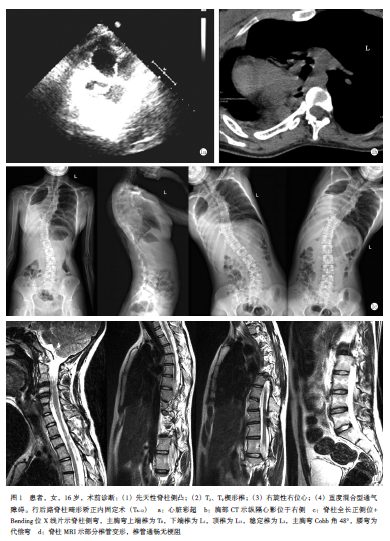
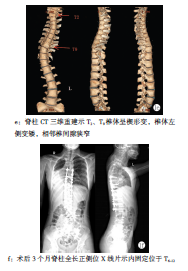
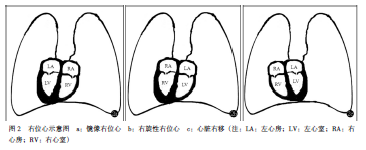
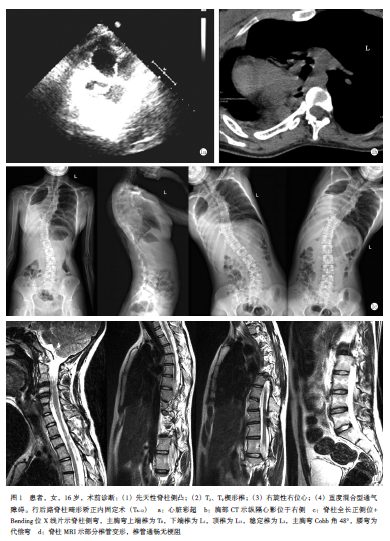
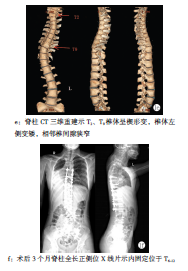
患者,女,16岁,因“活动后气促10余年,发现脊柱侧凸8余年”入本院。

17岁少年,身高仅153cm。背部高高隆起,让他无法正常行走。“我还能奔跑吗?”一个对普通人而言简单的动作,于他而言则是天大的心愿。一个月前,上海交通大学医学院附属新华医院骨科脊柱外科蒋雷生团队收治了这名藏族学生,展开脊柱侧后凸后路截骨矫形手术。目前,这名17岁的少年已经能像正常人一样行走了。蒋雷生主任提醒,脊柱侧弯是一个不断进展加重的疾病,一旦确诊,需尽早干预,不要等到非常严重了才去四处求医,这
本期共刊出了3篇有关脊柱特殊类型感染的论著和综述,其临床意义值得关注。这些文章涉及脊柱结核和脊柱布氏杆菌病,这两种脊柱特殊类型感染的发病率呈逐年上升趋势,已经成为需要引起重视和观察研究的健康问题。以脊柱结核为例,虽然前些年我国肺结核发病率呈下降趋势,但受人口增加、人口老龄化、耐药菌、人类免疫缺陷病毒(HIV)传播等现状的影响,全球结核病卷土重来,骨关节结核患者数量呈明显上升趋势。骨与关节结核是最常
脊柱骨折的搬运至关重要,学会正确的搬运方法,不仅能减轻患者的疼痛而且能有效避免损伤加重,减少并发症。
患者资料患者,男性,39岁,因“腰背部疼痛1年余加重伴双侧大腿部疼痛3个月余”入院
1 腰椎椎间盘突出症手术治疗 ✦保守治疗3月了吗? 大多数(70%)椎间盘突出患者保守治疗3月后,症状可完全消失。 手术适应证:①病史超过三个月,严格保守治疗无效或保守治疗有效,但经常复发且疼痛较重者;②首次发作,但疼痛剧烈,尤以下肢症状明显,患者难以行动和入眠,处于强迫体位者;③合并马尾神经受压表现;④出现单神经根麻痹,伴有肌肉萎缩、肌力下降;⑤合并椎管狭窄者。 2 腰椎间盘突出症融合手术


梅斯医学MedSci APP
医路相伴,成就大医
#脊柱侧凸#
42
谢谢分享学习
81
学习了
75
6666666
63
#先天性#
42
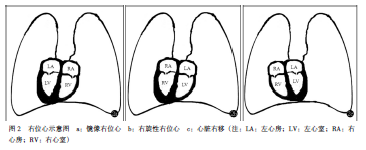
#右位心#
46
学习了
54