Arthroscopy:ACL重建术后感染**盥洗+清创
2014-06-30 紫川秀第二 丁香园
随着运动医学技术的发展,膝关节交叉韧带损伤接受治疗的患者数量越来越多,而前交叉韧带重建术后出现关节腔内的感染情况并不多见,但是一旦发生,其结果可能是灾难性的,文献报道其发生率在0.14%-1.7%之间,感染后主要的治疗措施是盥洗+清创,但关节腔内有内置物,上述治疗措施的有效性被一些学者质疑,为进一步明确交叉韧带重建术后膝关节感染行盥洗+清创对治疗这类疾病是否有效,美国学者进行了一项meta分析
随着运动医学技术的发展,膝关节交叉韧带损伤接受治疗的患者数量越来越多,而前交叉韧带重建术后出现关节腔内的感染情况并不多见,但是一旦发生,其结果可能是灾难性的,文献报道其发生率在0.14%-1.7%之间,感染后主要的治疗措施是盥洗+清创,但关节腔内有内置物,上述治疗措施的有效性被一些学者质疑,为进一步明确交叉韧带重建术后膝关节感染行盥洗+清创对治疗这类疾病是否有效,美国学者进行了一项meta分析,并将相关结论发表在Arthroscopy杂志上。
研究者使用5个检索平台进行了数据检索,包括MEDLINE,OVID,Medscape,Web of Science,Google scholar,筛选出前交叉韧带重建术后出现膝关节感染而行盥洗,清创的研究报道。

研究定义治疗失败的案例包括:因感染而最终需要移除移植物或者是进行交叉韧带翻修重建术的患者。
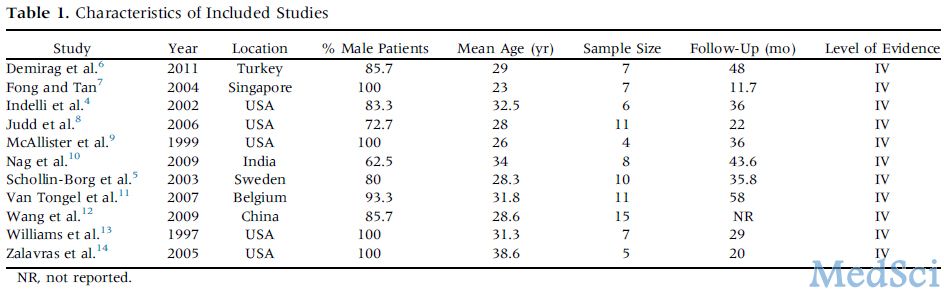
研究共纳入11个符合标准的研究(表1),共计90例患者,盥洗+清创治疗前交叉韧带重建术后膝关节感染的成功率为85.6%,其中约34.5%的患者需要多次手术治疗。而治疗失败,最终需要性后期前交叉韧带重建翻修的患者为14.4%(13例)。多因素分析显示,金黄色葡萄球菌感染,多次的盥洗+清创术,异体韧带移植等是感染后治疗失败的危险因素。
表1:纳入的相关研究
该研究提示前交叉韧带重建术后发生膝关节感染后,盥洗+清创术可以作为治疗的首选措施。较为激进的处置方法,如感染后行清创并植入物移除,除了治疗过程更为复杂,治疗时间更长之外,其对膝关节面上的软骨破坏也更为严重,最终可导致后期的膝关节骨关节炎发生。和激进的传统方法相比,单纯盥洗+清创具有以下优势:技术要求更低,手术时间更短,围手术期死亡率更小等。
作者推荐,对前交叉韧带损伤修复重建术后的患者,首选盥洗+清创治疗。
原始出处:本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#清创#
28
#ART#
21
#ROS#
31