小儿脑髓鞘的正常发育
2021-10-29 医学影像服务中心 医学影像服务中心
磁共振成像是目前对小儿脑髓鞘发育无创评估的最佳方法。小儿髓鞘形成过程比较复杂,必须了解髓鞘形成及其MRI影像表现。
哈尔滨医科大学附属第六医院
*哈尔滨医科大学附属第二医院
磁共振成像是评估脑髓鞘化最好的无创方式。常规T1和T2加权是对中枢神经系统髓鞘形成进行评估所必需的序列。了解MR成像中髓鞘形成的进展,在诊断小儿疾病包括白质营养不良、髓鞘发育不良和获得性脱髓鞘疾病是至关重要的。
图1.髓鞘示意图
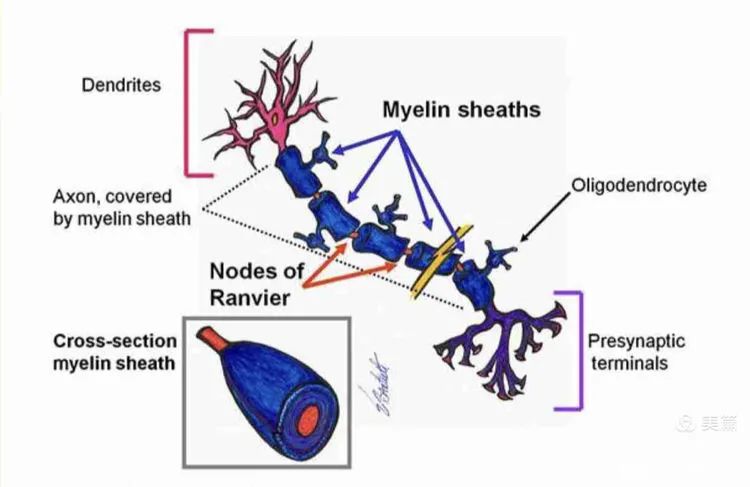
髓鞘是神经元的重要组成部分,髓鞘包裹轴突由郎飞结分割成片段(图1)。
图2.髓鞘形成过程特点
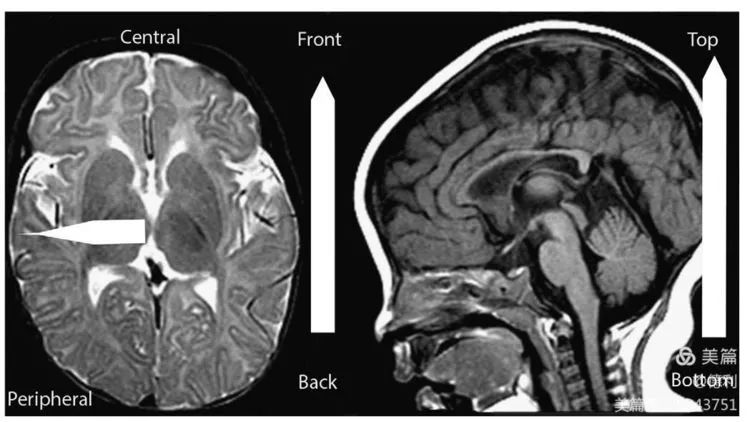
髓鞘的形成是一个动态的过程特点,脑白质各部分的成熟和髓鞘形成是有先后顺序的,脑白质髓鞘化的顺序是从脑的尾侧向头侧,从背侧向腹侧,先中央后外周,感觉纤维早于运动纤维(图2)。
图3A.新生儿出生就已经髓鞘化的结构(T1)
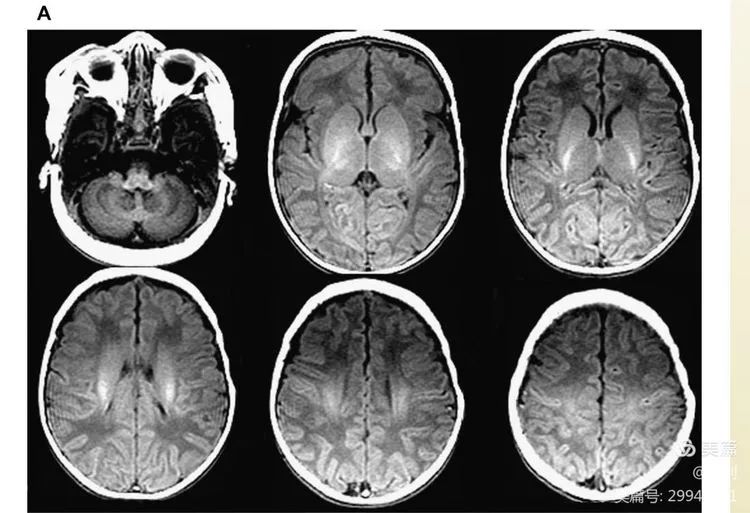
图3B.新生儿出生就已经髓鞘化的结构(T2)
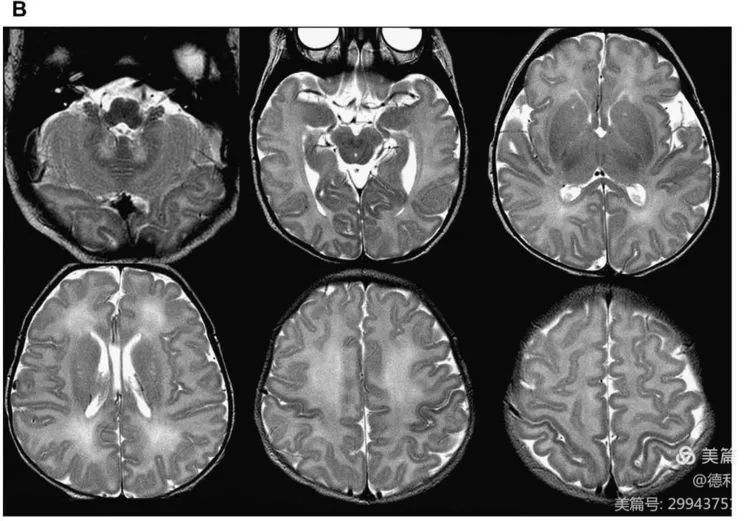
新生儿出生就已经髓鞘化形成的结构,表现为T1高信号T2低信号(图3A,B),包括内囊后肢、丘脑腹外侧、脑桥背侧、小脑上下脚、大脑脚、放射冠中央、中央回周围。
图4. 小儿 4个月的髓鞘
小儿4个月髓鞘的图像。4个月,内囊前肢T1上的轻微高信号,中央放射冠和半卵圆中心髓鞘增厚,胼胝体的压部髓鞘化。内囊的前肢在T2上没有髓鞘化的表现(图4)。
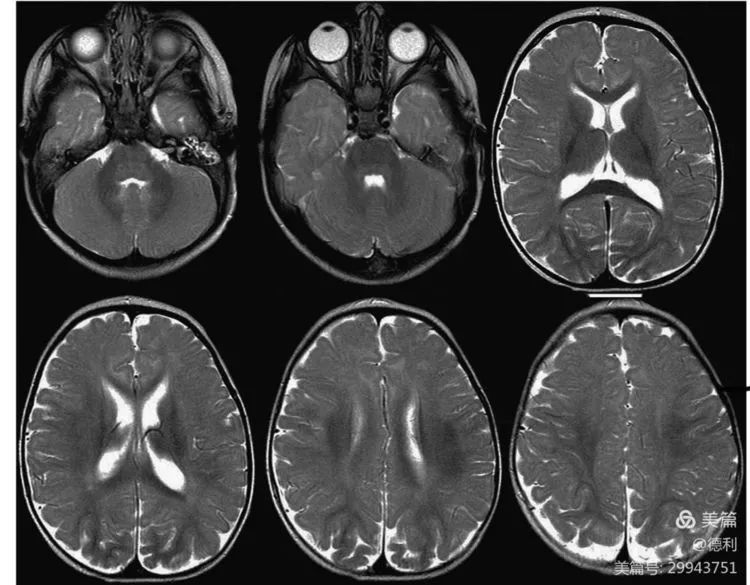
图5.小儿6个月的髓鞘

小儿6个月髓鞘的图像。6个月,髓鞘在中央白质,特别是在半卵中心和放射冠区域有大量增加。髓鞘形成在T1最明显,在T2滞后,内囊的前肢有一个轻微的T2低信号,胼胝体髓鞘增厚(图5)。
图6.小儿9个月的髓鞘

小儿9个月髓鞘的图像。9个月,T2髓鞘白质信号逐渐变低,内囊的前肢可见T2髓鞘化。T1髓鞘化进一步增厚、扩大(图6)。
图7.小儿12个月的髓鞘
小儿12个月髓鞘的图像。12个月,T1髓鞘形成基本完成,T2在半卵圆中心、放射冠以及胼胝体和内囊中有进一步的髓鞘增厚,额叶和颞叶仍然有相当数量的无髓鞘化白质(图7)。
图8.小儿18个月的髓鞘(T1)
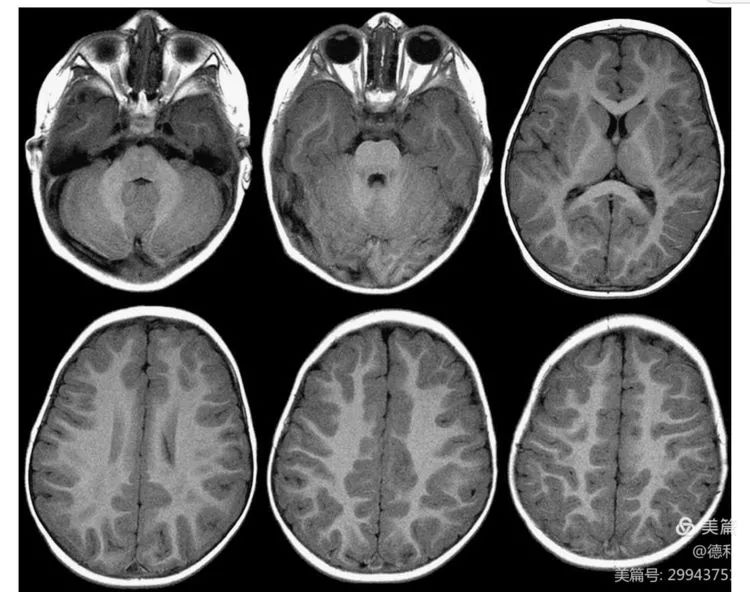
小儿18月T1髓鞘的图像。18个月,T1髓鞘完整,外观与12个月时相似。中央和深部白质进一步增厚和“膨胀”(图8)。
图9.小儿18个月的 髓鞘(T2)

小儿18个月T2髓鞘。T2除额下叶和颞叶以及周围区髓鞘终末区外,几乎有完整的髓鞘形成,如图9。
图10. 小儿2岁的髓鞘
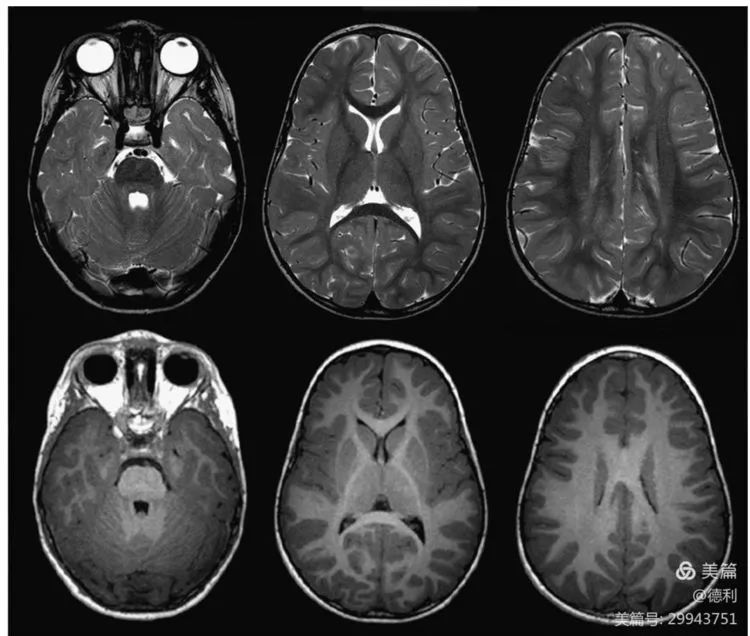
小儿2岁髓鞘的图像。2岁,T1和T2上的髓鞘形成完成,侧脑室旁、额下叶和颞叶可有部分T2高信号残留(图10)。
图11.小儿3岁的髓鞘
小儿3岁髓鞘的图像。3岁,T1加权和T2加权序列上,髓鞘是完整的和成人样的外观(图11)。
图12.轴向和冠状T2加权序列显示正常的髓鞘终末区
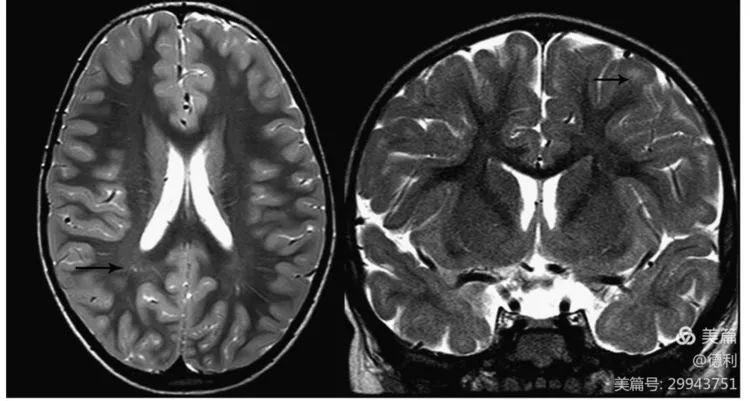
轴向和冠状T2加权序列显示正常的髓鞘终末区(黑色箭头)。这些区域通常位于后脑室周围区域以及额颞叶皮层下区域(图12)。
记忆对照卡片1: 胼胝体髓鞘形成
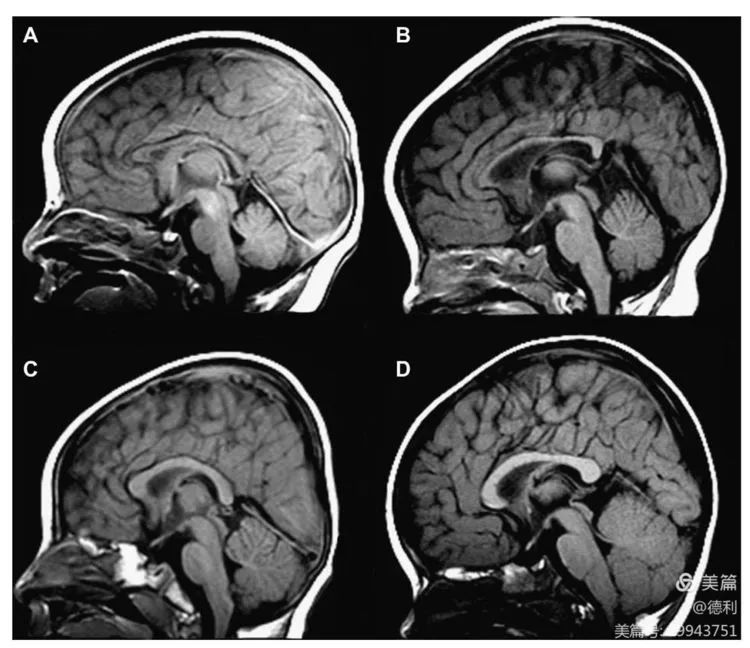
胼胝体髓鞘形成的图像。矢状T1加权序列显示胼胝体正常发育。(B) 4个月;(C) 6个月;(D) 16个月(见记忆卡片1)。
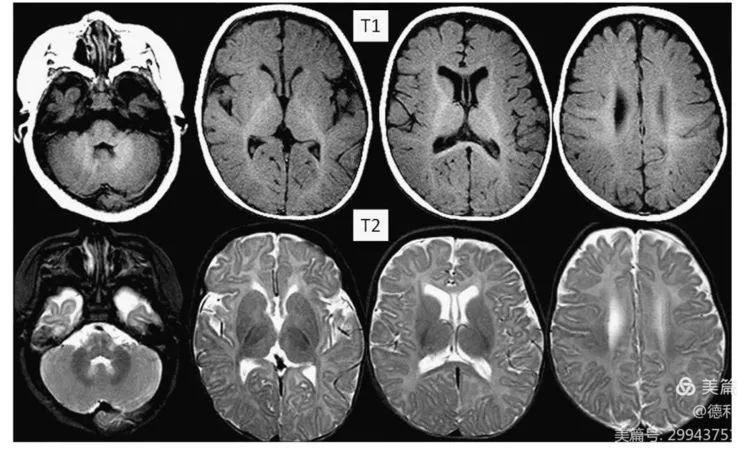
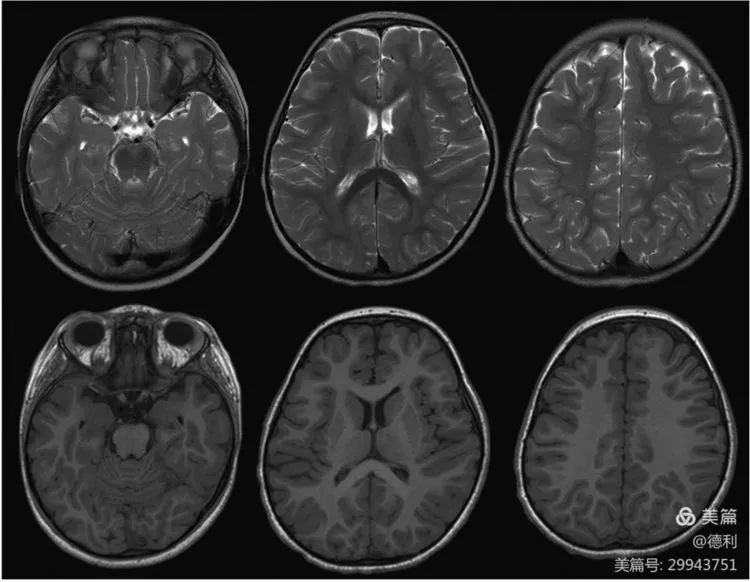
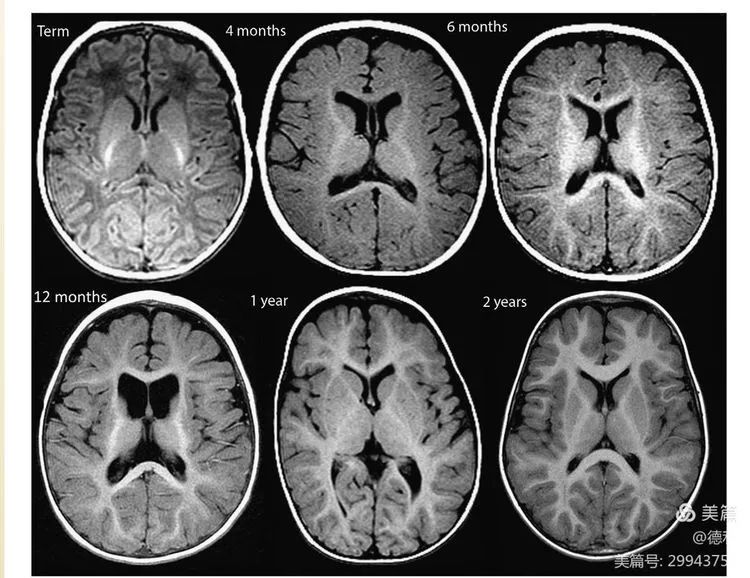
记忆对照卡片2: T2正常髓鞘形成进展
T2正常髓鞘形成进展。MR成像从出生(足月新生儿)到2岁正常髓鞘形成的T2加权序列(见记忆卡片2)。
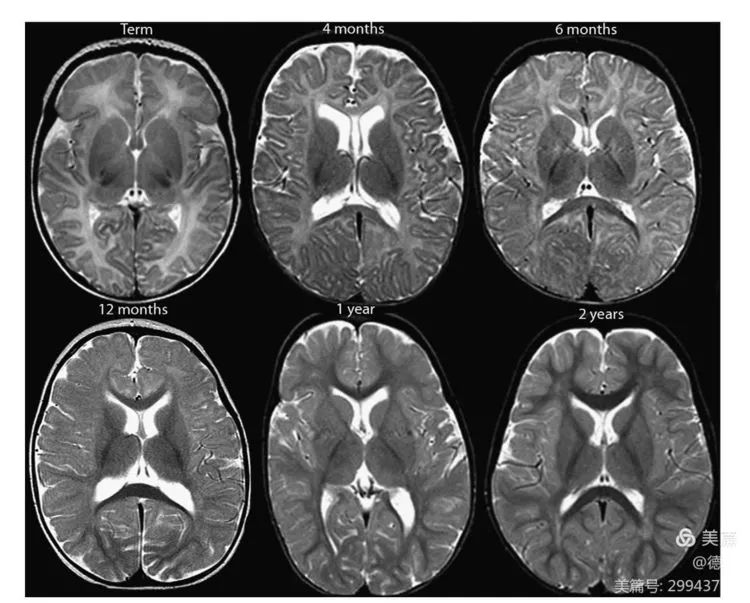
记忆对照卡片3: T1正常髓鞘形成进展
T1正常髓鞘形成进展。MR成像从出生(足月新生儿)到2岁正常髓鞘形成的T1加权序列(见记忆卡片3)。
磁共振成像是目前对小儿脑髓鞘发育无创评估的最佳方法。小儿髓鞘形成过程比较复杂,必须了解髓鞘形成及其MRI影像表现。此外,胼胝体发育的正常进展及对髓鞘形成的正常终末区的识别,牢记并收藏记忆卡片对于理解小儿脑髓鞘发育至关重要。
文献来源:Branson, HM; Normal myelination: a practical pictorial review.[J].Neuroimaging Clin N Am.2013,23(2):183-95.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#髓鞘#
60
#正常发育#
65
#发育#
65
好,受教了。
98
好,学习了
87