Cardiovasc Diabetol:动态血压与无症状糖尿病患者心功能障碍的相关性
2022-05-30 MedSci原创 MedSci原创
24小时动态血压与糖尿病患者的心室重塑、冠状动脉微血管功能障碍和舒张功能障碍显著相关。
2 型糖尿病 (T2D) 和高血压通常合并存在,与亚临床心肌结构和功能变化有关,这些改变使患者易患心血管疾病 (CVD),特别是心力衰竭的风险增加。本研究旨在明确在没有心血管疾病的 2 型糖尿病患者中,血压(BP)与左心室(LV)重塑、收缩/舒张功能和冠状动脉微血管功能之间的关联。
研究人员对 2 型糖尿病患者和年龄、性别及种族相匹配对照进行了全面的心血管表型分析,包括空腹血、经胸超声心动图、心血管磁共振成像以及办公室和 24 小时动态血压监测。通过多变量线性回归评估血压与 T2D 患者心室重塑和功能的成像标志物之间的独立相关性。
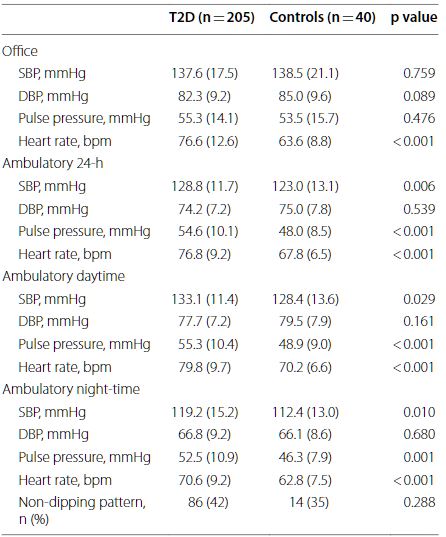
两组受试者的血压监测结果
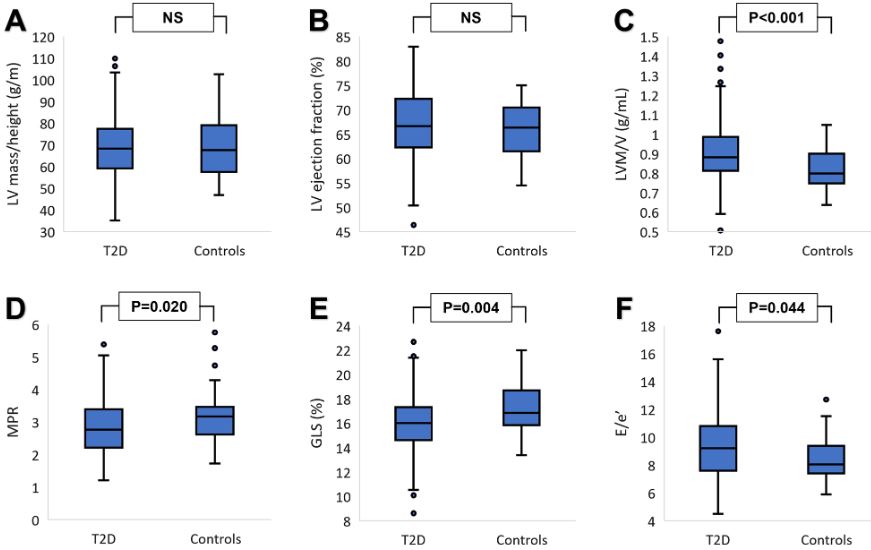
招募了 205 位 2 型糖尿病患者(平均 63±7 岁)和 40 位对照(平均 61±8 岁)。与对照组相比,2 型糖尿病患者的 24 小时平均收缩压明显更高(128.8±11.7 vs 123.0±13.1 mmHg,p=0.006),但办公室血压无此差异。与对照患者相比,2 型糖尿病患者更可能存在左心室向心性重塑(体积:0.91±0.15 vs 0.82±0.11 g/mL,p<0.001)、心肌灌注储备减少(2.82±0.83 vs 3.18±0.82, p=0.020)、收缩功能障碍(整体纵向应变:16.0±2.3 vs 17.2±2.1%, p=0.004)和舒张功能障碍(9.30±2.43 vs 8.47±1.53, p=0.044)。
两组受试者心脏参数的差异
在根据14个临床变量进行调整的多变量回归模型中,24 小时平均收缩压与左心室向心性重塑(β=0.165, p=0.031)、舒张功能障碍(β=0.273, p<0.001)和心肌灌注储备减少(β=-0.218, p=0.016)独立相关。此外,24 小时平均舒张压也与左心室向心性重塑相关(β=0.201, p=0.016)相关。
24 小时动态收缩压与心脏各参数的相关性
总而言之,24 小时动态收缩压与无症状 2 型糖尿病患者的心室重塑、冠状动脉微血管功能障碍和舒张功能障碍独立相关,但办公室血压无此相关性。
原始出处:
Yeo, J.L., Gulsin, G.S., Brady, E.M. et al. Association of ambulatory blood pressure with coronary microvascular and cardiac dysfunction in asymptomatic type 2 diabetes. Cardiovasc Diabetol 21, 85 (2022). https://doi.org/10.1186/s12933-022-01528-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
38
#相关性#
34
#ASC#
32
#BET#
39
#功能障碍#
40
#心功能#
47
#糖尿病患者#
33
#无症状#
32
#动态血压#
38
学习了
44