Lancet:大数据看中风的预防(INTERSTROKE试验)
2016-07-17 佚名 来宝网
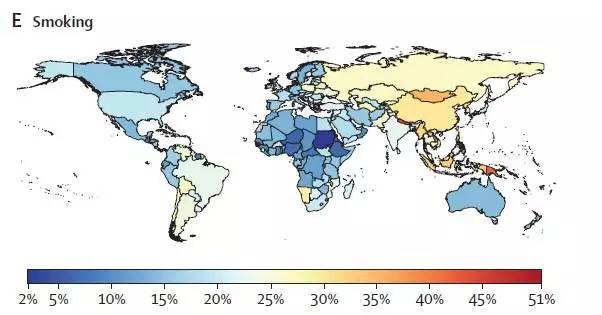
最近麦克马斯特大学的研究者称,全世界90%的中风,发病原因大致可以归结为10个,但是十个致病因素会因为地域的不同而所占的比例也有差别。近期发表在《柳叶刀》(The Lancet )杂志上的文章表明,中风的预防是目前中风最紧迫的事情,但是地域差异性会影响预防策略的实施。中风是引起死亡和残疾的主要原因,尤其是对于中低收入人群来说,中风的两种形式包括由于血栓引起的缺血性中风,大概占到85%;另外一种是脑
最近麦克马斯特大学的研究者称,全世界90%的中风,发病原因大致可以归结为10个,但是十个致病因素会因为地域的不同而所占的比例也有差别。
中风是引起死亡和残疾的主要原因,尤其是对于中低收入人群来说,中风的两种形式包括由于血栓引起的缺血性中风,大概占到85%;另外一种是脑出血引起的中风,占到总人数的15%。
由该研究机构Martin O'Donnell博士和Salim Yusuf博士主导的该研究与来自32个国家的科学家一道对22个国家的6000名受试者进行了研究,其中对主要对这10种中风的危险因素进行了评估,该项目被称为INTERSTROKE,受试者来自欧洲、亚洲。美洲、非洲以及大洋洲,通过对各种类型的人群进行调查,找到中风的主要原因。
PHRI 项目负责人O'Donnell 说:“该研究通过对世界主要地区和国家,分地区和范围的研究中风危险因素,我们已经发现约有90%的中风患者致病原因无非是这十个,同时研究也指出高血压是在这十种原因中最重要的一个,也是能够有效缓解中风最重要的靶标。”
调查者在观察不同危险因素的同时发现,如果危险因素消失,患病比例将会大大降低。
高血压消除后会减少48%,如果会多运动患病比例会降到36%,再加上合理的饮食会降到19%。
而且在这十种致病因素中也不是孤立存在的,比如说肥胖和糖尿病之间的密切联系,当同时有这两种致病因素时,中风的概率就更大了。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ERS#
28
#Lancet#
0
好文值得点赞!继续关注学习。
70
wonderful
32
有意义的大数据研究。
71
非常好的文章
91