Radiology:二尖瓣环CT形态与经导管主动脉瓣置换术后二尖瓣返流的关系
2021-08-23 shaosai MedSci原创
经导管主动脉瓣置换术(TAVR)是目前公认的治疗症状严重的主动脉瓣狭窄患者的最佳术式之一。在接受TAVR治疗的患者中,约有25%的患者存在中至重度的二尖瓣反流,且大部分患者均未接受规范化治疗。
 经导管主动脉瓣置换术(TAVR)是目前公认的治疗症状严重的主动脉瓣狭窄患者的最佳术式之一。在接受TAVR治疗的患者中,约有25%的患者存在中至重度的二尖瓣反流,且大部分患者均未接受规范化治疗。关于TAVR术后二尖瓣反流的改善率和改善预测因素,现存文献中研究结果存在矛盾。
经导管主动脉瓣置换术(TAVR)是目前公认的治疗症状严重的主动脉瓣狭窄患者的最佳术式之一。在接受TAVR治疗的患者中,约有25%的患者存在中至重度的二尖瓣反流,且大部分患者均未接受规范化治疗。关于TAVR术后二尖瓣反流的改善率和改善预测因素,现存文献中研究结果存在矛盾。
经胸超声心动图(TTE)和经食道超声心动图是评估二尖瓣解剖结构的常规检查手段。然而,由于二尖瓣解剖结构的复杂性、超声心动图对操作者的依赖性以及经食道超声心动图的半侵袭性,仅用超声心动图评估TAVR术后二尖瓣反流的原因和改善预测因素是具有挑战性的。因此,使用多层CT(MSCT)对行TAVR患者的二尖瓣进行评估的趋势越来越显著。目前,MSCT已被纳入TAVR评估的常规流程中。由于传统的马鞍形二尖瓣环的投影面积超出了实际的二尖瓣环,因此临床上提出了一种新的基于MSCT的D形二尖瓣环模型,并在接受二尖瓣置换术的患者中进行了相关的研究,但还未在接受TAVR且合并二尖瓣反流的患者中进行系统评价。
近日,发表在Radiology杂志的一项研究通过使用MSCT根据D型二尖瓣环的测量,探讨了TAVR术后中重度二尖瓣反流的原因、改善程度和改善预测因素,为临床准确评估TAVR术后患者预后提供了影像学支持。
本项研究评估了2012年4月至2019年10月期间接受TAVR的528名连续患者。排除了曾接受主动脉瓣置换术的患者和中度或重度二尖瓣狭窄的患者,最终共有104名中度至重度二尖瓣反流患者符合纳入标准并被纳入最终分析。二尖瓣反流的严重程度至少降低一个等级被认为是TAVR后二尖瓣反流改善的标志。评估了TAVR后长达5年的二尖瓣反流改善的随访情况。使用专用的后处理软件,在MSCT上评估二尖瓣环的尺寸(环面积、周长、三尖瓣与三尖瓣之间的距离、瓣膜间距离和前后距离)和环的钙化,并探讨了与TAVR后二尖瓣反流改善的关系。
本研究共纳入104名接受TAVR的二尖瓣反流患者(平均年龄74岁±7岁;61名男性)。在TAVR术后,79名患者的二尖瓣反流得到改善,其余25名患者的二尖瓣反流保持不变。在TAVR后的第一年改善最大。D型二尖瓣环参数,包括环周长(几率[OR],1.05;95%CI:1.01,1.1;P = .02)和三尖瓣对三尖瓣(OR,1.2;95%CI:1.03,1.39;P = .02)以及瓣膜间距离(OR,1.15;95%CI:1.02,1.31;P = .02)都与二尖瓣反流改善有关。此外,冠心病患者在TAVR后二尖瓣反流的改善程度更高(OR,0.17;95%CI:0.04,0.76;P = .02)。原发性二尖瓣反流(OR,5.1;95%CI:1.1,24;P = .04)和D型环周长(OR,1.06;95%CI:1,1.11;P = .04)是TAVR后二尖瓣反流改善较少的独立预测因素。
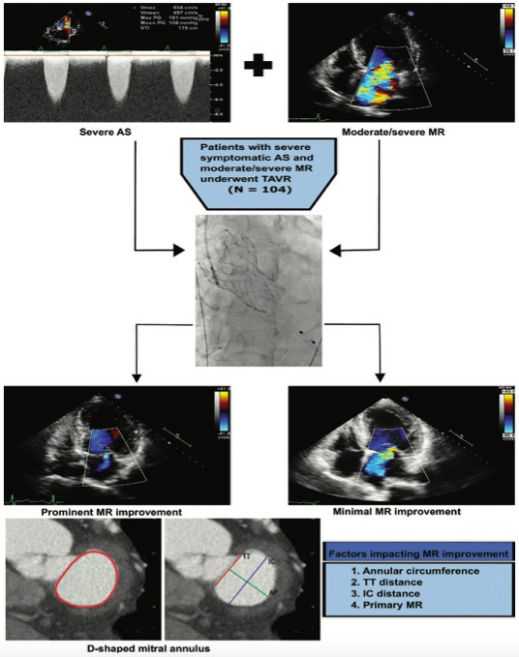
图 对该研究进行了总结。AS=主动脉瓣狭窄,IC=瓣间,MR=二尖瓣反流,PG=压力梯度,TAVR=经导管主动脉瓣置换术,TT=三尖瓣-三尖瓣,Vmax=最大主动脉速度,Vmean=平均主动脉速度,VTI=速度时间积分。
本研究发现,在接受经导管主动脉瓣置换术(TAVR)的患者中,合并中度至重度二尖瓣反流是十分常见的表现之一,且经常不被重视因此很少进行常规治疗。同时,在TAVR术前采用简化的D形瓣环方法对二尖瓣解剖进行分析,确定瓣环周长和原发性二尖瓣反流是TAVR术后二尖瓣反流改善较少的独立预测因素。除了确定二尖瓣反流的原因外,在MSCT上对合并中重度二尖瓣反流的TAVR候选者进行简化D型瓣环尺寸的评估是十分简便且可重复的,并有助于预测TAVR后二尖瓣反流的预后,从而有利于临床术前治疗方案的准确制定,并确定潜在的经皮二尖瓣介入治疗与TAVR的可行性。
原文出处:
Xi Li,Abdullah Hagar,Xin Wei,et al.The Relationship of Mitral Annulus Shape at CT to Mitral Regurgitation after Transcatheter Aortic Valve Replacement.DOI:10.1148/radiol.2021210267
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#置换#
42
#主动脉瓣#
33
#主动脉瓣置换术#
31
#主动脉#
33
#二尖瓣返流#
39
#二尖瓣#
33
#经导管#
30
#经导管主动脉瓣置换#
39
#置换术#
40