Nature:肿瘤的斯德哥尔摩综合症
2017-10-12 路人丙 中美药源
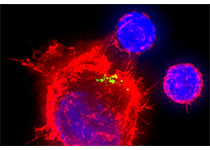
今天的《自然》杂志发表一篇荷兰科学家关于耐药肿瘤对肿瘤药物依赖的工作(doi:10.1038/nature24037)。作者发现四种不同 BRAF V600E 变异恶黑肿瘤细胞用 BRAF 抑制剂 dabrafenib 和 MEK 抑制剂 trametinib 处理 3 - 5 个月后出现耐药株,但如果突然停止用药这些耐药株会大量死亡,说明这些肿瘤细胞对 BRAF 和 MEK 抑制剂产生依赖。作者
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#斯德哥尔摩综合症#
39
#Nat#
34
好好看下.内容丰富
50
很好的专题,值得品味及分享
52
学习了新知识
50