JGH:无症状胆总管结石会增加内镜下逆行胰胆管造影后胰腺炎的发生率
2022-02-13 MedSci原创 MedSci原创
胆囊结石 其症状取决于结石的大小和部位,以及有无阻塞和炎症等。部分胆囊结石患者终身无症状,即所谓隐性结石
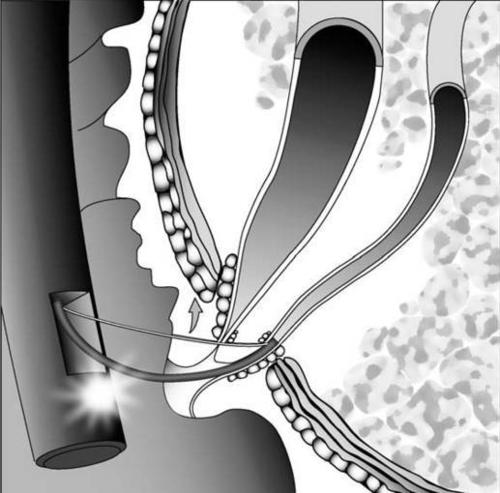
胆总管结石(CBD)是全世界常见的健康问题。由于CBD可导致胆道相关的并发症,包括急性胆管炎和胆汁性胰腺炎,因此,临床上通常建议患者通过内窥镜逆行胰胆管造影(ERCP)进行内窥镜治疗。然而,ERCP是一种技术上比较困难的手术,并且有很高的手术相关并发症的风险。在ERCP相关的并发症中,ERCP后胰腺炎(PEP)是最常见和最严重的并发症,其发生率3%-10%。考虑到CBD结石是一种良性疾病,确定CBD结石切除后发生PEP的风险因素对于降低PEP的发生率至关重要。本项研究的目的是探究急性胆管炎是否是 CBD 结石患者 PEP 的临床危险因素。

为了完成本项研究,研究人员进行了一项多中心回顾性调查,将 1539 名患者分为无急性胆管炎组和有急性胆管炎组。然后使用一比一的倾向评分匹配来比较两组之间 PEP 的发生率,以调整 PEP 的潜在混杂因素。最后通过相关性分析进行了差异分析。
研究结果发现在整个队列中,没有和有急性胆管炎患者的 PEP 发生率分别为 9.6%(52/542)和 1.8%(18/997)(P< 0.001,OR= 5.8)。在倾向匹配队列中,没有和有急性胆管炎患者的 PEP 发生率分别为 8.3% (27/326) 和 2.5% (8/326)(P= 0.002,OR= 3.6)。在调整PEP的混杂因素后,非急性胆管炎患者的PEP发生率显着高于急性胆管炎患者。

图:无症状胆管炎与胰腺炎的发生的关系
本项研究证实当 CBD 结石去除后,急性胆管炎可能是 PEP 的重要临床危险因素。对于没有急性胆管炎的患者,内镜医师应仔细解释 PEP 的具体风险,并积极实施 PEP 的预防措施。
原始出处:
Hirokazu Saito. Et al. Increased post-endoscopic retrograde cholangiopancreatography pancreatitis for choledocholithiasis without acute cholangitis.Journal of Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#发生率#
46
#内镜#
50
#无症状#
48
#造影#
60
#胆总管结石#
0
#胆管#
46