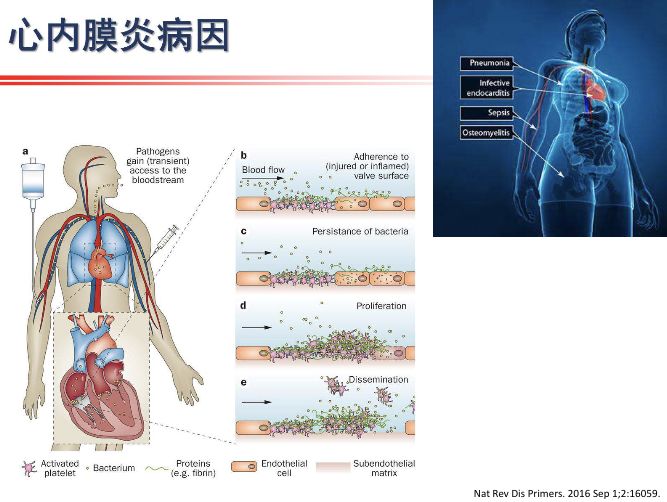
JACC:BAV或MVP感染性心内膜炎:到底是否需抗生素预防?
2018-07-20 吴星 环球医学
关于二尖瓣主动脉瓣(BAV)或二尖瓣脱垂(MVP)患者感染性心内膜炎(IE)的信息很少。目前,不推荐感染性心内膜炎抗生素预防(IEAP)用于这些病症。2018年6月,发表在《J Am Coll Cardiol》的一项研究描述BAV和MVP患者IE的临床和微生物学特征,并将其与合并或不合并IEAP指征的IE患者进行比较,以确定IEAP在这些疾病中的潜在益处。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#感染性#
24
#内膜#
21
#JACC#
28
#ACC#
28
#心内膜炎#
36