Pharmacol Res:常添加在茶叶中的中药吴茱萸或可导致严重心律失常
2018-05-04 朱柳媛 中国循环杂志
欧洲研究人员发现,广泛使用的一种中药——吴茱萸(evodia rutaecarpa)中含有能导致心律失常的成分。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





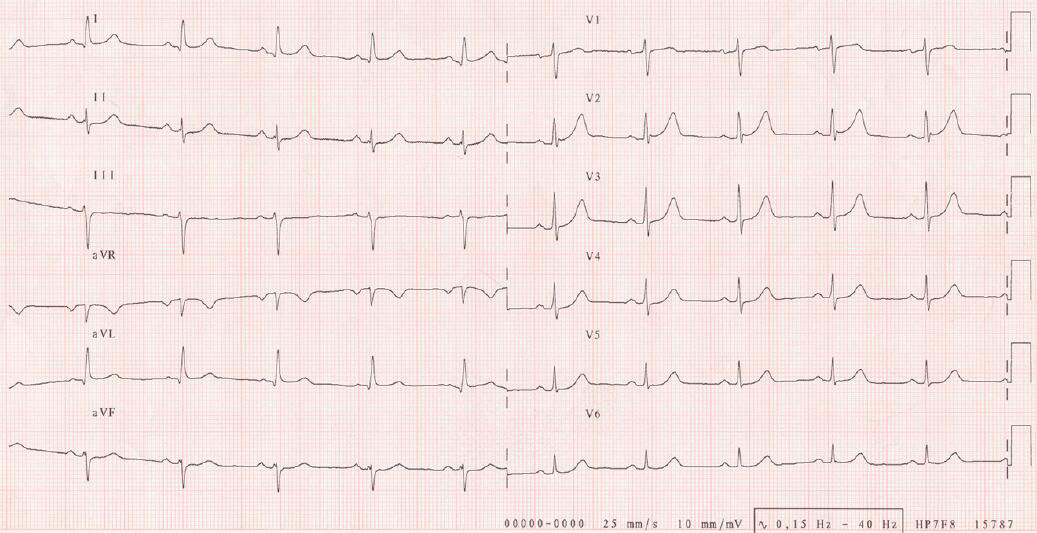





#吴茱萸#或可导致严重#心律失常#,但是对于慢心律而言,吴茱萸可能改善心率,它具有一定的强心作用。
163
#Pharm#
39
#pharma#
46
#Pharmacol#
44
#MAC#
38
学习了谢谢分享!
82
学习了.谢谢分享
56
学习了谢谢分享!!
79
#茶#
35
了解一下谢谢
69