JACC:心血管医师需终身学习 在职教育体系怎样改进?
2018-03-08 闫盈盈 环球医学网
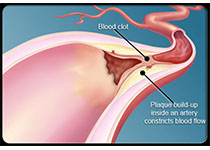
人们都说“活到老,学到老”,学习不仅是每个人终其一生应该坚持的习惯,对医生这一特殊群体而言,更是不断提升医术、精进业务的一大法宝。心血管疾病是全球的头号死因,在2012年死于该疾病的人数占总数的31%。考虑到心血管医师的职业培养是卫生建设的重中之重,2018年1月,发表在《J Am Coll Cardiol》的一项美国研究,探索了心血管医师终身学习的教育新体系。
终身学习对于执业心血管医师而言非常重要。目前,终身学习的机制停滞不前,不能满足执业心血管医师的需求。随着心血管疾病负担和患者护理复杂性的增加,以及非临床任务的压力,发展教育规划成为满足当代心血管职业需求的必然。终身学习设备需要囊括现代、实用教育工具的模式转变。在毕业后的医学教育中,新的教育策略方面的新证据支持医师职业生涯不同阶段有望广泛应用这些工具。在这个来自培训部领导委员会研究员的评论中,作者提出了3种新的教育工具:个性化学习、适应性学习和翻转课堂,以改善终身学习,满足受训人员对执业心血管医师相关方面的教育需求。
心血管医学是一门复杂的科学,需要医师们在临床中不断摸索并学习新知识、get新技能,只有完善医师的职业培训才能更好地为心血管病人保驾护航!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
24
#终身学习#
25
#ACC#
33
学习谢谢分享
59