Ann Neurol:血脑屏障破坏与阿尔茨海默氏症和血管疾病的关系
2021-05-27 MedSci原创 MedSci原创
这些结果提供了早期证据,表明BBB破坏与AD和血管风险均相关,但其效应可通过空间尺度加以区分。BBB对小分子的通透性对认知功能具有更大的影响。
血脑屏障(BBB)破坏被认为是人类认知障碍的早期生物标志物。但是,BBB破坏与脑部病理(最常见的是阿尔茨海默氏病和血管疾病)之间的关联仍然知之甚少。
近日,神经病学领域权威取杂志Annals of Neurology上发表了一篇研究文章,这项研究旨在两个分子水平上测量了轻度认知障碍(MCI)患者的BBB功能,特别是BBB对水和白蛋白分子的通透性。

该研究纳入了55名老年参与者,其中包括33名MCI患者和22名对照者。研究人员使用一种新的MRI技术测量了BBB对水的通透性,并使用CSF/血清白蛋白比率确定BBB对白蛋白的通透性。认知表现通过区域特定的综合评分进行评估。研究人员评估了AD病理(包括CSFAβ和ptau)与血管危险因素之间的相关性。
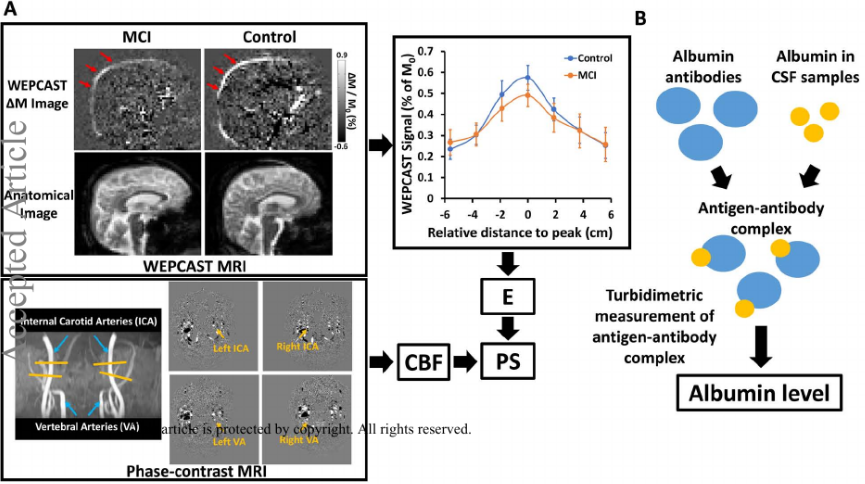
BBB功能评价
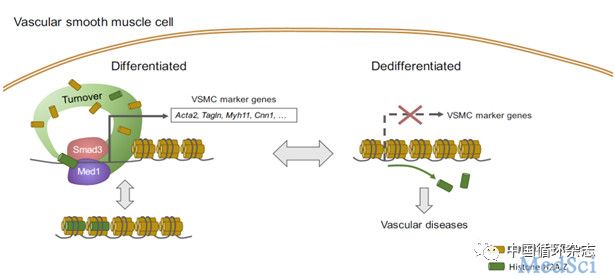
与认知正常的受试者相比,MCI患者的BBB对小分子(如水)的通透性增加,但对大分子(如白蛋白)的通透性却未增加。研究人员发现BBB对水的通透性与CSF中AD标记Aβ和ptau水平有关。另一方面,研究人员发现BBB对白蛋白的通透性与血管危险因素尤其是高胆固醇血症有关,但与AD病理学无关。研究人员发现BBB对小分子而非大分子的通透性可预测认知功能。
这些结果提供了早期证据,表明BBB破坏与AD和血管风险均相关,但其效应可通过空间尺度加以区分。BBB对小分子的通透性对认知功能具有更大的影响。
原始出处:
B.S. Zixuan Lin,et al.Blood-brain barrier breakdown in relationship to Alzheimer and vascular disease.Annals of Neurology.2021.https://onlinelibrary.wiley.com/doi/10.1002/ana.26134
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#阿尔茨#
43
#阿尔茨海默氏#
57
#阿尔茨海#
54
#Neurol#
52
#血脑屏障#
59
#阿尔茨海默#
36
#血管疾病#
54
优秀
74
好
69