Neurology:孤立性脑桥受累的亚急性硬化性全脑炎
2018-07-29 zyx 神经科病例撷英拾粹
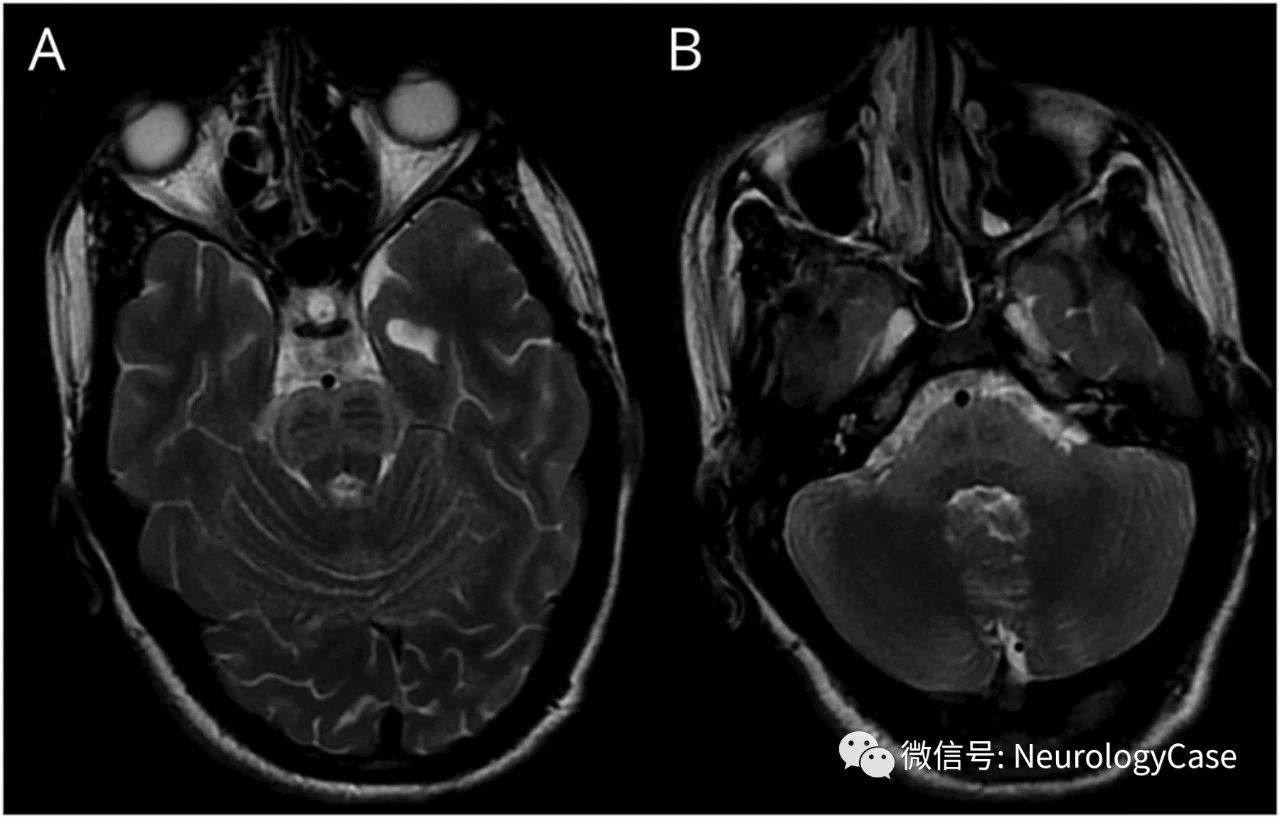
16岁男孩,4岁时罹患麻疹,出现全面性肌阵挛性抽搐和进行性认知和感觉功能下降6月余。脑电图可见全面性,周期性,高幅放电(图1),脑脊液抗麻疹免疫球蛋白G抗体滴度为212.33U/mL(正常8U/mL),提示亚急性硬化性全脑炎(SSPE)。头颅MRI可见腹侧脑桥和小脑中脚孤立性T2高信号(图2)。
16岁男孩,4岁时罹患麻疹,出现全面性肌阵挛性抽搐和进行性认知和感觉功能下降6月余。脑电图可见全面性,周期性,高幅放电(图1),脑脊液抗麻疹免疫球蛋白G抗体滴度为212.33U/mL(正常8U/mL),提示亚急性硬化性全脑炎(SSPE)。头颅MRI可见腹侧脑桥和小脑中脚孤立性T2高信号(图2)。尽管予以对症治疗,但患儿仍在3周时死于心脏骤停。SSPE患者的头颅MRI通常表现为大脑皮质和脑室周围白质受累。脑干病变罕见,先前仅有一例孤立性受累的病例报道。早期脑干受累可能提示侵袭性病程。
(图1:脑电图提示全面性,周期性的,刻板的,高幅尖波和慢波发放,持续1-2秒,每5-7秒出现一次)
(图2:脑MRI可见腹侧脑桥[A,B]和双侧小脑中脚[B]T2WI高信号)
原始出处:Kumar N1, Ranjan A2, Kumar A2, Kumar B2. Teaching NeuroImages: Isolated pontine involvement in subacute sclerosing panencephalitis. Neurology. 2018 Jul 17;91(3):e293-e294.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Neurol#
29
#脑桥#
27
#脑炎#
18
#硬化性#
30
#孤立性#
26
Case report,学习了。
0