Circ Cardiovasc Interv:PCI治疗放射相关CAD的死亡率研究
2016-06-29 Mechront 译 MedSci原创
与标准的动脉粥样硬化性冠心病(CAD)患者相比,既往外照射治疗的CAD患者进行冠状动脉冠状动脉介入术(PCI)后,其短期和长期的死亡风险均增加。克利夫兰诊所心脏和血管研究所的Milind Y. Desai博士和同事对314名连续PCI治疗的患者进行了观察性研究。患者分两组:体外放射治疗的CAD组(EBRT;n = 157)和以前没有EBRT曝光的CAD患者(对照组;n = 157)。研究以全因死亡
与标准的动脉粥样硬化性冠心病(CAD)患者相比,既往外照射治疗的CAD患者进行冠状动脉冠状动脉介入术(PCI)后,其短期和长期的死亡风险均增加。
克利夫兰诊所心脏和血管研究所的Milind Y. Desai博士和同事对314名连续PCI治疗的患者进行了观察性研究。患者分两组:体外放射治疗的CAD组(EBRT;n = 157)和以前没有EBRT曝光的CAD患者(对照组;n = 157)。研究以全因死亡率为主要终点;心血管疾病死亡率为次要终点。
在平均随访6.6年后的年内,发生了101例死亡。EBRT组和对照组分别为59(59%)例和42 (42%)例(P = .04)。多变量Cox比例风险模型显示,以前的EBRT和全因死亡率存在持续性的关联,并且是独立的(HR = 1.85; 95% CI, 1.21-2.85)。
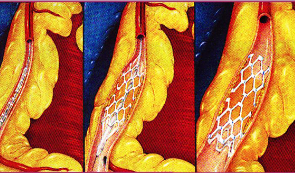
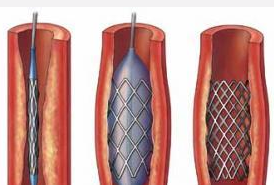
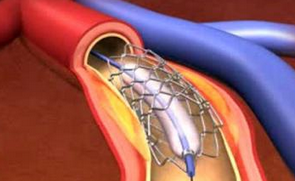
其他独立增加全因死亡率的因素包括球囊血管成形术或BMS置入位置 vs.DES置入位置(HR = 2.5; 95% CI, 1.61-3.97)、SYNTAX得分至少11(样本中位数;HR = 1.99;95% CI,1.32-3.04)、心功能III级或IV级(HR = 1.83;95% CI,1.15-2.91)、吸烟史(HR,1.88;95% CI,1.1-3.09)和年龄65岁以上(HR = 1.7;95% CI,1.07-2.07)。
69例患者发生了心血管疾病死亡,EBRT组和对照组分别为37 (54%)例和32 (46%)例。此外,EBRT组63%的死亡(n = 37)被确定为相关的心血管疾病原因。调整年龄、性别、NYHA心功能III级或IV级、SYNTAX得分和PCI类型后的非匹配分析显示,以前的EBRT暴露是心血管死亡率的持续性独立预测因子(aHR = 1.7; 95% CI, 1.06-2.89)。
研究结果表明,既往EBRT为PCI术后全因死亡率和心血管死亡的独立危险因素。
原始出处:
Reed GW, et al. Long-Term Mortality in Patients With Radiation-Associated Coronary Artery Disease Treated With Percutaneous Coronary Intervention.Circ Cardiovasc Interv. 2016;doi:10.1161/CIRCINTERVENTIONS.115.003483.
Radiation-associated CAD confers increased mortality risk after PCI.Healio.June 28, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASC#
29
#PCI治疗#
37
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
57
很好,不错,以后会多学习
64
己拜读,受益匪浅
0