Neurology: 脑电图和经颅多普勒生物标志物联合应用对迟发性脑缺血的预测效果良好!
2021-12-06 Naomi MedSci原创
迟发性脑缺血(DCI)是蛛网膜下腔出血(SAH)的主要并发症。 脑电图和经颅多普勒生物标志物联合应用对DCI的预测效果最好。临床变量与EA、大脑中动脉高血流速度的结合可以改善预测模型效果。
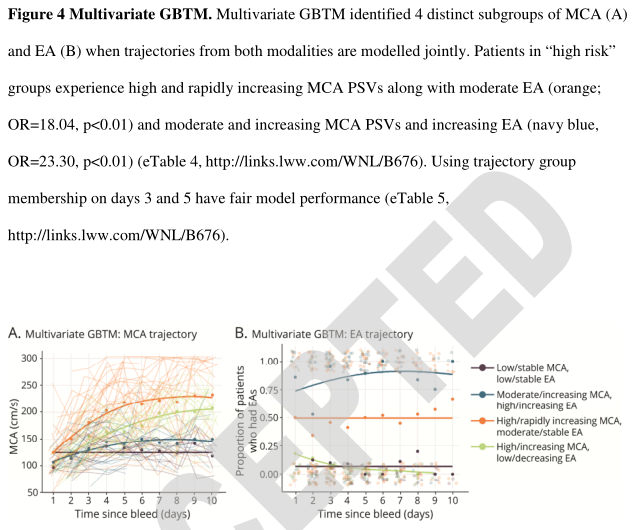
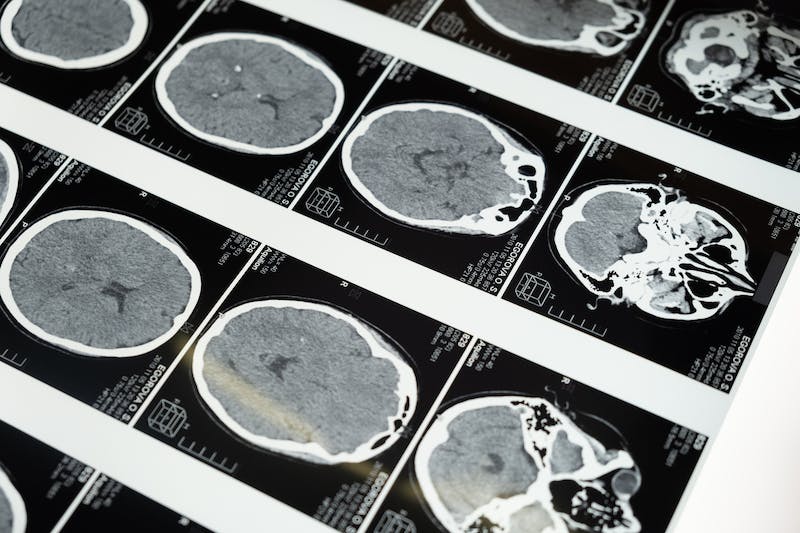
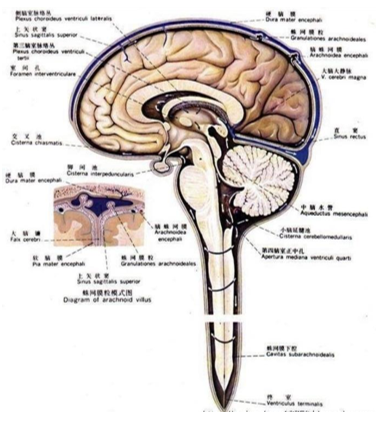
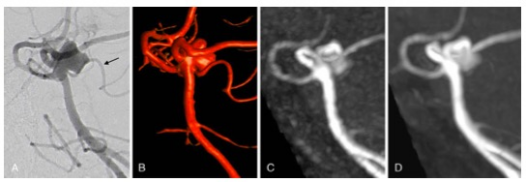
迟发性脑缺血(DCI)是蛛网膜下腔出血(SAH)的主要并发症。过去人们认为DCI完全是由大血管痉挛引起的,因此经颅多普勒超声(TCD)目前是DCI监测的标准。虽然TCD是一种无创、便携的床边监测检查,但它不能频繁进行(每天最多1-2次),且取决于操作员,并可能受到患者解剖结构的限制(较差的颞骨窗口),还可能受到其他生理参数(如心率和血压)的影响。此外,当前观点认为仅靠血管痉挛并不能完全解释DCI。
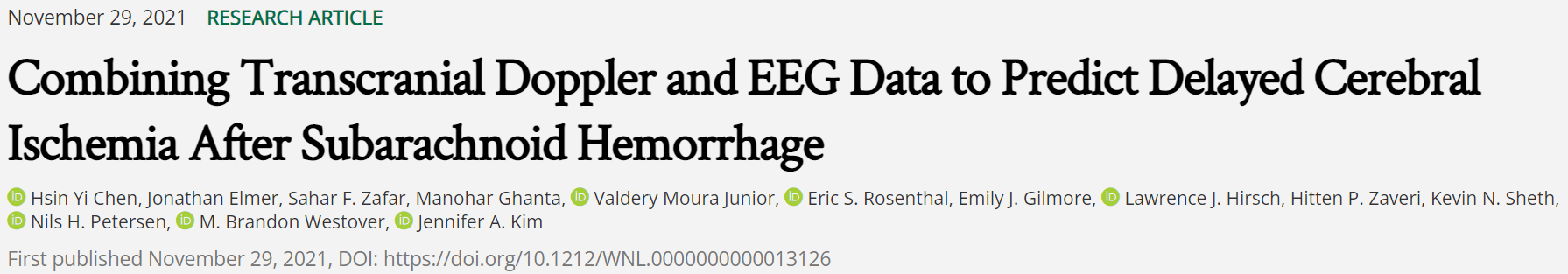
连续脑电图(CEEG)已成为DCI预测的一种有前途的辅助诊断工具,解决了TCD监测的一些局限性。CEEG是一种非侵入性的便携设备,最重要的是可以提供数天的连续数据。研究表明定量CEEG测量,如相对α变异性和刺激后α/δ比和癫痫样异常(EA)与DCI相关。也有证据表明,患者通常在发生DCI之前首先表现出CEEG改变,而且EEG与DCI的相关性比TCD速度升高更强。TCD和CEEG关于DCI风险的存在潜在协同信息。然而,TCD和CEEG数据对DCI预测的联合效用尚未得到评估。
近日,有研究人员试图解决联合TCD和CEEG测量是否可以识别SAH后的DCI。假设在单个模型中结合TCD和CEEG参数将比单独使用任何一种模式都能改善DCI预测。
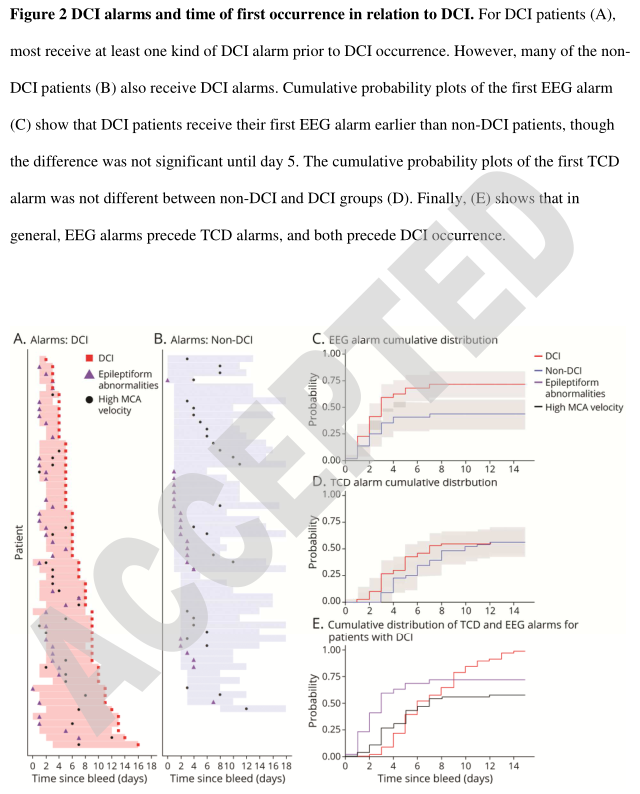
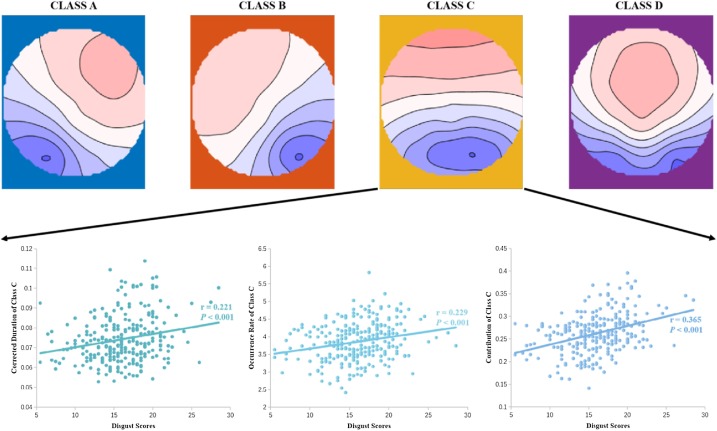
研究回顾性评估了中-重度蛛网膜下腔出血(2011-2015,Fisher=3-4或Hunt-Hess=4-5)的患者,这些患者在住院期间都有预期的TCD和EEG采集。每天记录大脑中动脉(MCA)收缩期峰值速度(PSV)和痫样异常(EA)的存在或不存在,包括癫痫发作、痫样放电和节律/周期活动。使用Logistic回归分析确定EA和TCD预测DCI的显著协变量。基于群体的轨迹建模(GBTM)被用来通过识别与DCI风险相关的MCA、PSV和EA的不同群体轨迹来解释随时间的变化。
- 评估了107名患者,其中56名(51.9%)发展为DCI。DCI的单变量预测因子是在第3天或之前均存在大脑中动脉高血流(PSV≥200 cm/s,Se=27%,Sp=89%)和电针(Se=66%,Sp=62%)。
- 电针预测DCI的两个单变量GBTM轨迹(Se=64%,Sp=62.75%)。使用经颅多普勒(TCD)和脑电图(EEG)监测的Logistic回归和GBTM模型表现更好。
- 最好的Logistic回归模型和GBTM模型同时使用TCD和EEG数据、入院时Hunt-Hess评分和动脉瘤治疗作为DCI的预测因素(Logistic回归:SE=90%,Sp=70%;GBTM:SE=89%,Sp=67%)。
脑电图和经颅多普勒生物标志物联合应用对DCI的预测效果最好。临床变量与EA、大脑中动脉高血流速度的结合可以改善预测模型效果。这些结果提示TCD和cEEG是预测DCI的有前景的互补监测手段。该模型有可能成为蛛网膜下腔出血管理的决策支持工具。
本研究提供了TCD和EEG联合监测可以识别蛛网膜下腔出血后迟发性脑缺血的II类证据。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#联合应用#
37
#标志物#
32
#迟发性脑缺血#
37
#Neurol#
33
学习
37
#迟发性#
64
学习了
52
学习了
53
学习了
38
很实用
41