Rheumatology:可溶性鸟苷酸环化酶刺激促进血管生成并钝化系统性硬化内皮细胞的肌成纤维细胞样特征
2022-07-31 紫菀款冬 MedSci原创
探索药物性可溶性鸟苷酸环化酶(sGC)刺激对系统性硬化(SSc)真皮微血管内皮细胞(SSc MVEC)受损血管生成和肌成纤维细胞样特征的影响。
目的:在系统性硬化(SSc)中,血管生成障碍与不同来源的肌成纤维细胞协调的纤维化发展[包括内皮-间充质转化(EndoMT)]同步进行。可溶性鸟苷酸环化酶(sGC)刺激对SSc皮肤成纤维细胞和小鼠模型显示出抗纤维化作用。
该研究旨在探索药物性sGC刺激对SSc真皮微血管内皮细胞(SSc MVEC)受损血管生成和肌成纤维细胞样特征的影响。
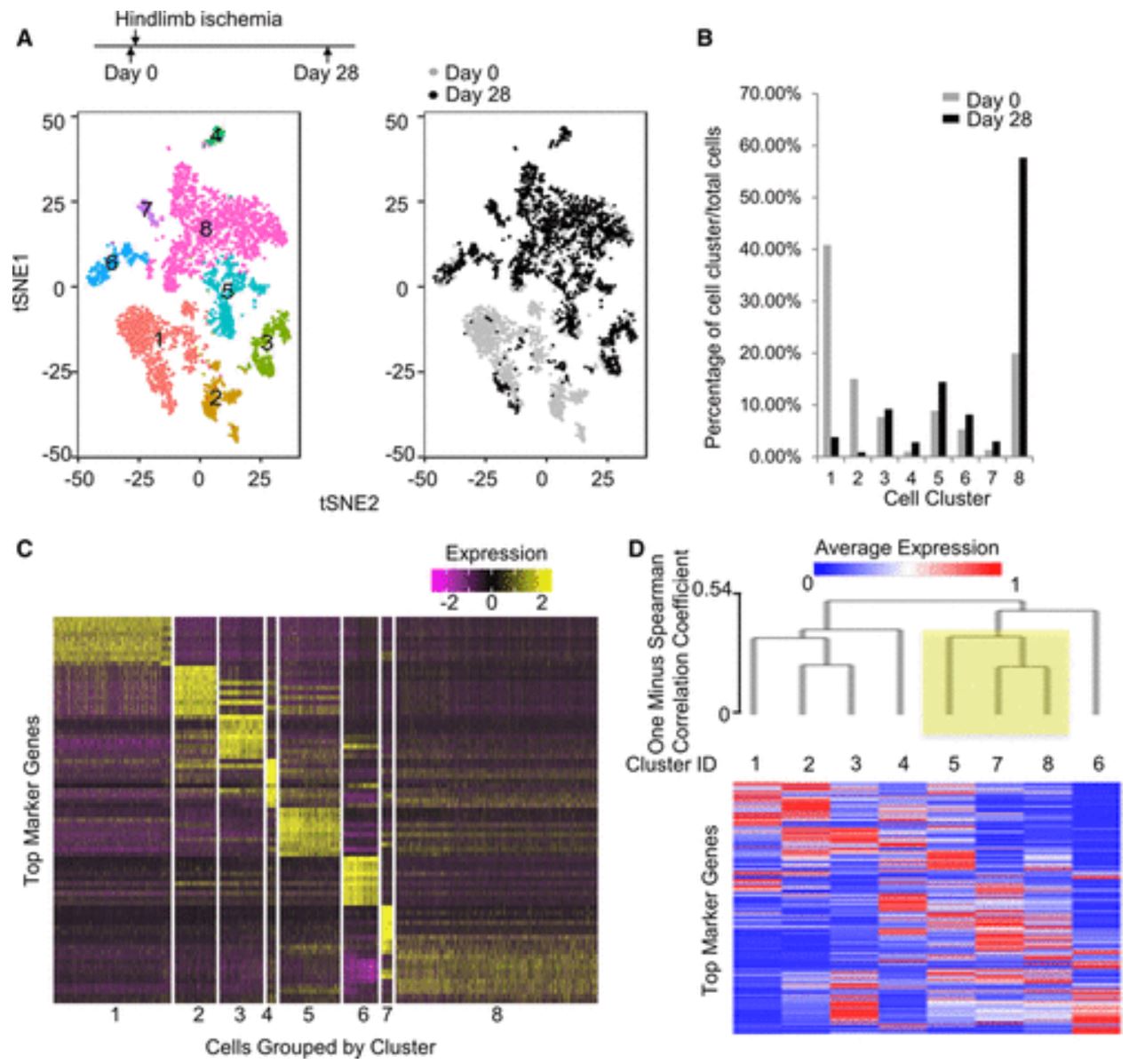
方法:用sGC刺激剂(sGCS)MK-2947刺激SSc MVEC和健康皮肤MVEC(H-MVEC),并用annexin V/PI流式细胞术和WST-1检测sGC刺激是否影响细胞活力/增殖。
研究血管生成和内皮细胞增殖,对MK-2947处理的SSc-MVEC进行伤口愈合和毛细血管形态发生分析,并分析内皮细胞/肌成纤维细胞标记物的表达和收缩能力。
结果:MK-2947治疗不影响H-MVEC活性/增殖,但显著增加了SSc-MVEC增殖、伤口愈合能力和血管生成能力。MK-2947治疗后,SSc MVEC表现出显著的促血管生成MMP9增加,抗血管生成MMP12和PTX3基因表达降低。
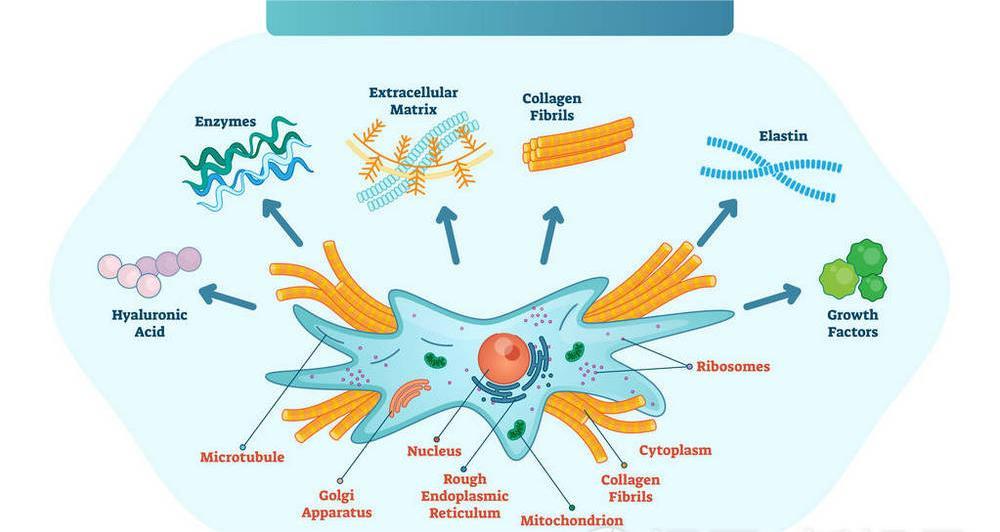
在MK-2947处理的SSc MVEC中,CD31和血管内皮钙粘蛋白的表达显著增加,同时α-平滑肌肌动蛋白、S100A4、I型胶原和Snail1间充质标记物的减少。此外,用MK-2947刺激sGC可显著抵消SSc MVEC收缩胶原凝胶的内在能力,并降低磷酸化ERK1/2蛋白水平。
结论:该研究结果首次表明,药物性sGC刺激有效地改善了SSc MVEC的血管生成性能,并钝化了肌成纤维细胞样促纤维化表型,从而为sGCSs用于SSc提供了新的证据。
文献来源:
Romano E, Rosa I, Fioretto BS, et al. Soluble guanylate cyclase stimulation fosters angiogenesis and blunts myofibroblast-like features of systemic sclerosis endothelial cells [published online ahead of print, 2022 Jul 28]. Rheumatology (Oxford). 2022;keac433. doi:10.1093/rheumatology/keac433
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Rheumatology#
50
#系统性#
38
#肌成纤维细胞#
47
#成纤维细胞#
60
#纤维细胞#
55
#系统性硬化#
53