CLIN CANCER RES:PI3K和BRAF联合抑制治疗晚期BRAF V600突变实体肿瘤
2018-01-08 MedSci MedSci原创
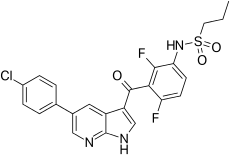
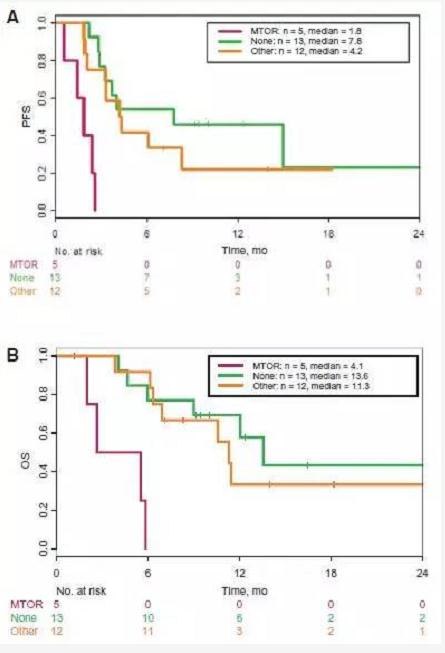
PI3K/AKT/mTOR通路与许多实体肿瘤有关,且被认为是BRAF抑制耐药的机制之一。因此,对BRAF V600突变的肿瘤,PI3K抑制剂与BRAF抑制剂联合治疗成为一种可行方案。CLIN CANCER RES近期发表了一篇文章,评估口服平PX-866联合每天2次Vemurafenib的安全性以及这一治疗策略的潜在预测性标志。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




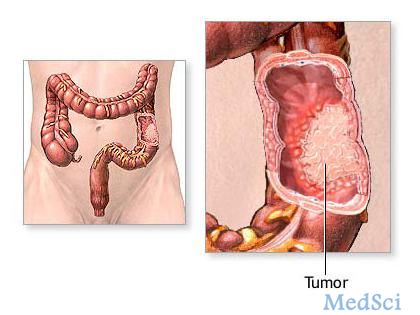
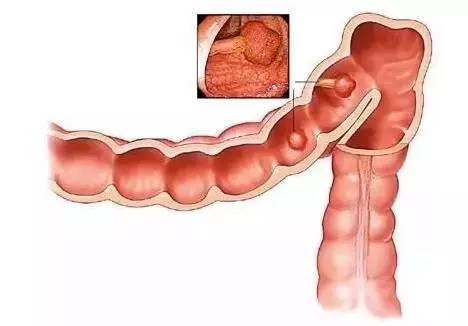
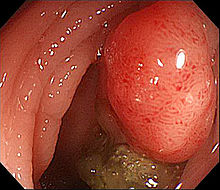




联合抑制治疗晚期.
51
#PI3K#
32
#BRAF#
40
#实体肿瘤#
30
阅
52
学习
43
阅
43
阅
36