J Clin OncoL:BRAF突变mCRC再细分,新突变亚型引人瞩目
2017-08-14 佚名 肿瘤瞭望
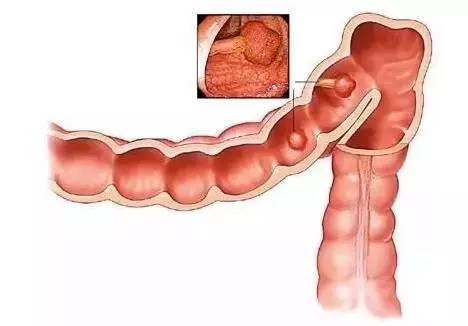
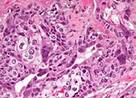
随着人们对转移性结直肠癌(mCRC)的遗传和分子改变的认识越来越深,转移性结直肠癌的临床实践也发生了重大的变革。例如,对于mCRC患者进行RAS和V600E BRAF突变检测已经成为普遍的共识,且有文献支持评估这类患者是否存在微卫星不稳定性(错配修复缺陷)和HER2扩增等。这些突变在转移性结直肠癌的临床管理中具有重要的指导意义,在不久的将来,分子分型共识亚型和免疫亚型也将推动某些治疗干预措施和策略
【1】Jones JC, Renfro LA, Al-Shamsi HO et al. Non-V600 BRAF mutations define a clinically distinct molecular subtype of metastatic colorectal cancer. J Clin Oncol
【2】Eric Van Cutsem and Jeroen Dekervel.Not All BRAF-Mutant Metastatic Colorectal Cancers Are Identical: Distinct Clinical Consequences of non-V600BRAF Mutations.J Clin Oncol
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CRC#
39
#mCRC#
44
#Oncol#
46
学习了,谢谢分享
69
#BRAF#
37
#BRAF突变#
36
V600EBRAF的预后较差,更容易出现腹膜转移,尽管实施各种化疗干预后患者的总生存期仍然较短。此外,V600EBRAF突变患者对于抗EGFR治疗反应有限,最新的指南不建议在这类患者中使用抗EGFR抗体。
72
研究最多的就是RAS基因的突变,几乎一半的转移性结直肠癌患者携带这种突变。已经明确的是,RAS突变患者对EGFR抑制剂无效。
66
学习了,谢谢。
76