OMERACT超声倡议:SpA和PsA中以共识为基础的附着点炎超声定义与评分的可靠性
2018-10-17 MedSci MedSci原创
Balint PV等研究者在2018年8月3日在Annals of the Rheumatic Diseases上在线发表一篇研究,旨在基于共识的超声定义评估脊椎关节炎(SpA)和银屑病关节炎(PsA)中附着点炎基本病变的可靠性,并评估其中哪些对附着点炎的定义和评分的影响最大。 该研究由11名超声医师对来自5例SpA/PsA患者4处两侧位置的40个附着点进行评价。对9个超声基本病变进行了二元评分
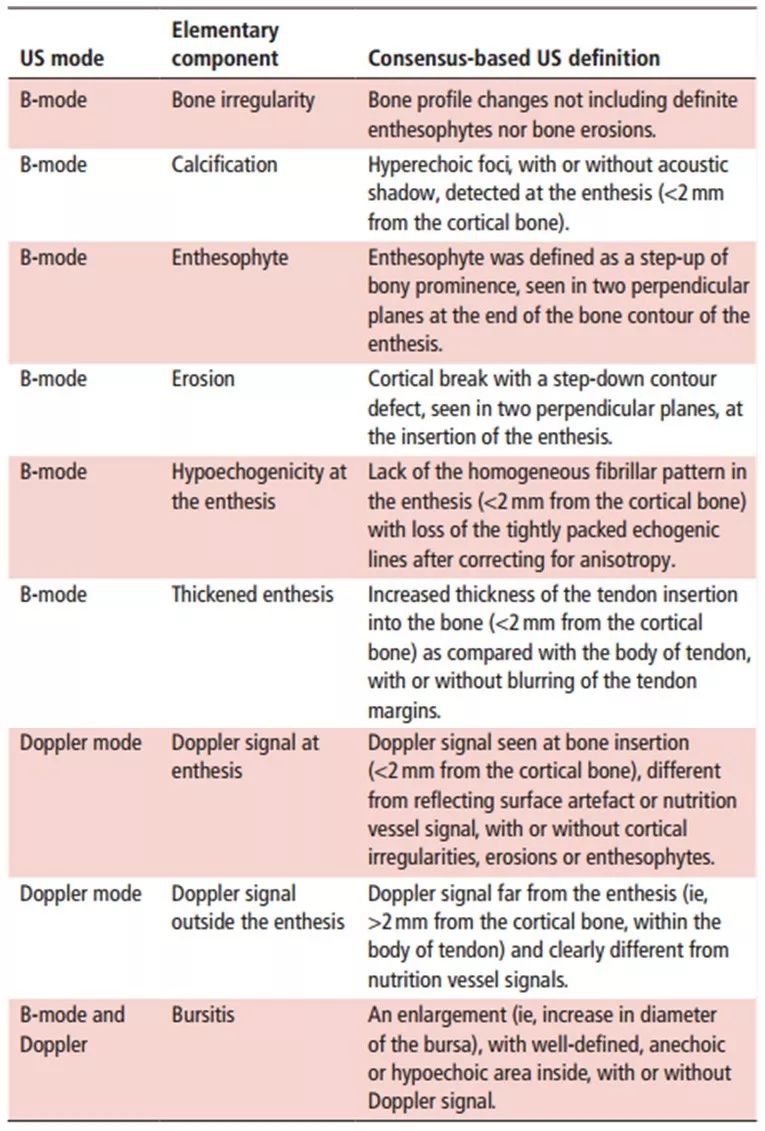
Balint PV等研究者在2018年8月3日在Annals of the Rheumatic Diseases上在线发表一篇研究,旨在基于共识的超声定义评估脊椎关节炎(SpA)和银屑病关节炎(PsA)中附着点炎基本病变的可靠性,并评估其中哪些对附着点炎的定义和评分的影响最大。 该研究由11名超声医师对来自5例SpA/PsA患者4处两侧位置的40个附着点进行评价。对9个超声基本病变进行了二元评分:低回声、肌腱插入增厚、边缘骨刺、钙化、侵蚀、骨不规则、滑囊炎、以及附着点炎内部和周围的多普勒信号(表1)。使用Kappa统计数据评估可靠性。并要求超声检查医师说明哪些病变可考虑为炎症性或结构性,以及应纳入针对附着点炎的最终定义中。仅将由至少75%的评估者认为是附着点炎的病变纳入最终的定义。 研究结果显示,除了边缘骨刺(55%)和骨不规则(54%)外,检出病变的患病率非常低。可靠性范围从低至高不等[增厚性附着点炎最低(kappa 0.1,95%CI:0~0.7),边缘骨刺最高(kappa 0.6,95%CI:0.5~0.7)]。当低患病率被调整后,所有病变的kappa值均增加,在肌腱插入(0.9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ERA#
31
#附着点炎#
46
#SpA#
27
#PSA#
38