Nature:揭示肿瘤抑制基因LATS控制人乳腺细胞命运机制
2017-01-10 佚名 生物谷
乳腺癌为何产生?某些乳腺癌病人如何对常规疗法产生抵抗性?在一项新的研究中,来自瑞士巴塞尔大学的研究人员对乳腺组织中这些分子过程获得新的认识。他们鉴定出肿瘤抑制基因LATS在乳腺癌产生和治疗中发挥着关键性的作用。相关研究结果于2017年1月9日在线发表在Nature期刊上,论文标题为“The Hippo kinases LATS1 and 2 control human breast cel
所有的乳腺癌都不是同样产生的。在高达70%的乳腺癌中,它们都有雌激素受体(estrogen receptor, ER)。如今,这些雌激素受体阳性乳腺癌能够相对较好地加以治疗。这些癌症需要雌激素才能生长,因此雌激素受体是许多药物的靶标。这些药物干扰雌激素表达、结合到雌激素受体上或者加快它的降解。
然而,大约三分之一的病人并不对药物治疗作出反应,或者说产生抵抗性。迄今为止,准确地预测哪些人对这种治疗作出反应是不可能的,这是因为其内在的分子机制仍然未得到充分的理解。
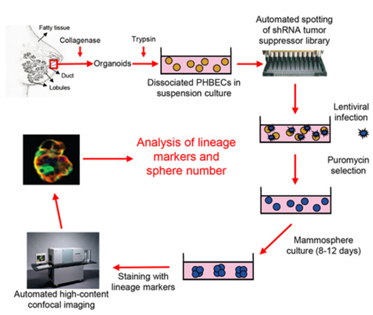
如今,在这项新的研究中,巴塞尔大学生物医学系的Mohamed Bentires-Alj教授团队鉴定出LATS在这种过程中发挥着重要的作用。他们能够证实这种酶通过与其他的蛋白协作,如何影响乳腺癌的产生和治疗。
肿瘤抑制基因LATS决定着细胞命运
研究人员着重关注阻止正常的细胞发生癌变的肿瘤抑制基因。特别地,他们研究了肿瘤抑制基因LATS1和LATS2。一旦剔除基因LATS,乳腺组织中的这些过程就会发生变化。
在缺乏LATS的情形下,乳腺上皮组织中的管腔前体细胞(luminal precursor cell)的数量增加了。人类大多数乳腺癌类型就起源自这类细胞。Bentires-Alj解释道,“LATS平衡着乳腺组织中的细胞命运。在它不存在时,这种平衡发生变化:更多的导致肿瘤产生的细胞产生了。”
抵抗降解
在健康的乳腺组织中,LATS携带着雌激素受体α(ERα)一起进入蛋白降解复合物中。若没有LATS,这种受体不再被正确地降解,而这对癌症治疗带来不利的后果。Bentires-Alj说,“我们能够证实缺乏LATS的乳腺癌细胞不再对氟维司群(Fluvestrant)作出反应,这意味着它们产生抵抗性。氟维司群是一种雌激素受体拮抗剂,促进雌激素受体降解。”
移除LATS也会让蛋白YAP和TAZ稳定化。YAP和TAZ在很多癌症中上调表达,促进细胞增殖。Bentires-Alj总结道,“鉴于我们对健康乳腺组织中的这些过程获得的新认识,我们如今也更好地理解癌症的起源细胞如何增殖,以及为何某些癌症抵抗治疗。”
Adrian Britschgi, Stephan Duss, Sungeun Kim, Joana Pinto Couto, Heike Brinkhaus, Shany Koren, Duvini De Silva, Kirsten D. Mertz, Daniela Kaup, Zsuzsanna Varga, Hans Voshol, Alexandra Vissieres, Cedric Leroy, Tim Roloff, Michael B. Stadler, Christina H. Scheel, Loren J. Miraglia, Anthony P. Orth, Ghislain M. C. Bonamy, Venkateshwar A. Reddy & Mohamed Bentires-Alj.The Hippo kinases LATS1 and 2 control human breast cell fate via crosstalk with ERα.Nature.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抑制基因#
28
#肿瘤抑制#
36
#ATS#
37
#Nat#
31