关于调整抗新型冠状病毒药物PF-07321332/利托那韦片(Paxlovid)适应症等内容的通知
2022-03-23 国家卫生健康委 网络
300mg奈玛特韦片与100mg利托那韦片同时服用,每12小时一次,连续服用5天。
3月23日,国家卫生健康委发布关于调整抗新型冠状病毒药物PF-07321332/利托那韦片(Paxlovid)适应症等内容的通知,具体内容如下:
各省、自治区、直辖市及新疆生产建设兵团卫生健康委、中医药管理局:
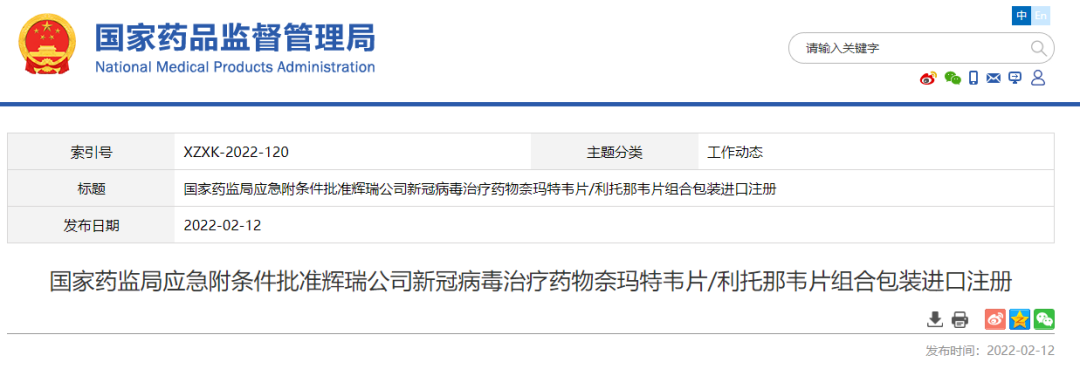
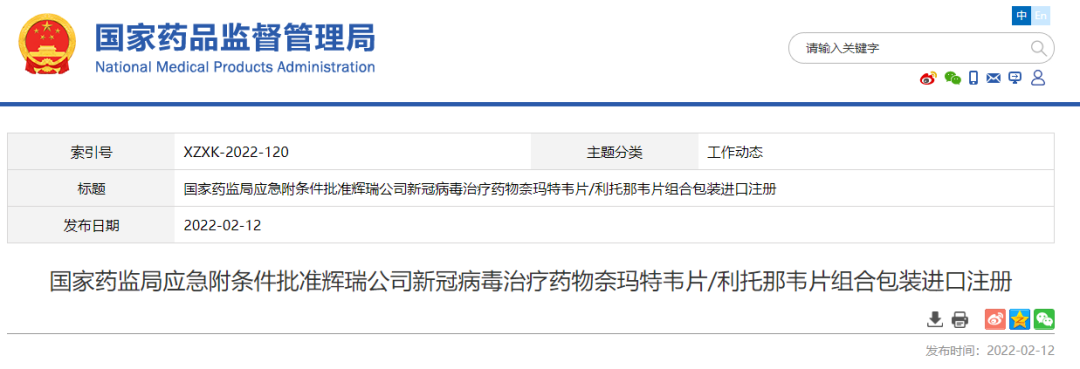
根据国家药品监督管理局批准奈玛特韦片/利托那韦片组合包装时核准的说明书,现对《新型冠状病毒肺炎诊疗方案(试行第九版)》抗病毒治疗中“PF-07321332/利托那韦片(Paxlovid)”相关内容调整如下:
一、药物名称
药物名称调整为“奈玛特韦片/利托那韦片组合包装”。
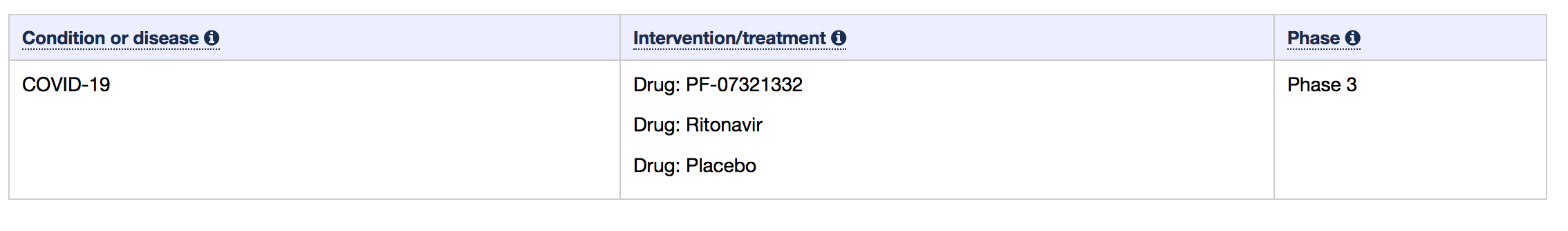
二、适应症
适应症为发病5天以内的轻型和普通型且伴有进展为重症高风险因素的成人。
三、用法用量
300mg奈玛特韦片与100mg利托那韦片同时服用,每12小时一次,连续服用5天。
四、禁忌症
对本品中的活性成份或任何辅料过敏的患者禁用。本品不得与高度依赖CYP3A进行清除且其血浆浓度升高会导致严重和/或危及生命的不良反应的药物联用。
使用该药品前应详细阅读国家药品监督管理局核准的《奈玛特韦片/利托那韦片组合包装说明书》,按照说明书规定的适应症、用法用量、剂量正确使用药品,对禁忌症、不良反应、药物的相互作用等情况要熟知,并详细询问患者的药物过敏史等情况,避免有禁忌症的患者使用该药品,避免与本品禁止联用的药品联用;各地要严格按照《药品不良反应报告和监测管理办法》要求,做好不良反应监测和报告工作,切实保证用药安全。
国家卫生健康委办公厅
国家中医药管理局办公室
2022年3月23日
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抗新型冠状病毒药物#
46
#适应症#
52
#利托那韦#
54
#利托那韦#
48
学习
47