Lancet Oncol:曲妥珠单抗+帕妥珠单抗±紫杉醇降级治疗HER2+/HR-早期乳腺癌
2022-04-20 Nebula MedSci原创
曲妥珠单抗+帕妥珠单抗±紫杉醇治疗12周后获得病理完全缓解的患者可获得很好的生存率
自2012年起,HER2阳性早期乳腺癌的(靶向)治疗策略得到了极大的优化。目前已探索了多种降级新辅助策略,以病理完全缓解作为替代终点来减少化疗的使用。本文汇报了WSG-ADAPT-HER2+/HR-试验的5年生存数据,并分析了病理完全缓解、早期治疗缓解和分子亚型的影响。
WSG-ADAPT-HER2+/HR-试验是一项由研究者发起的、多中心、开放标签、随机的2期研究,招募了年满18岁、组织学确诊、单侧、原发性浸润性、激素受体阴性和HER2阳性、非炎症性早期乳腺癌患者,随机(5:2)分成两组,接受曲妥珠单抗(首剂 8 mg/kg,随后 6 mg/kg·3周)+帕妥珠单抗(首剂 840 mg/kg,随后 420 mg/kg·3周)或曲妥珠单抗+帕妥珠单抗+紫杉醇(80 mg/m2·周)。主要终点是手术时的病理完全缓解率。
2014年3月3日至2015年10月6日期间,共招募了134位患者,随机分至两组:二联组 92位,三联组 42位。中位随访了59.9个月。治疗组间的无侵袭性疾病生存期、无复发生存期、局部无复发生存期、远处无病生存期和总生存期均无显著差异。
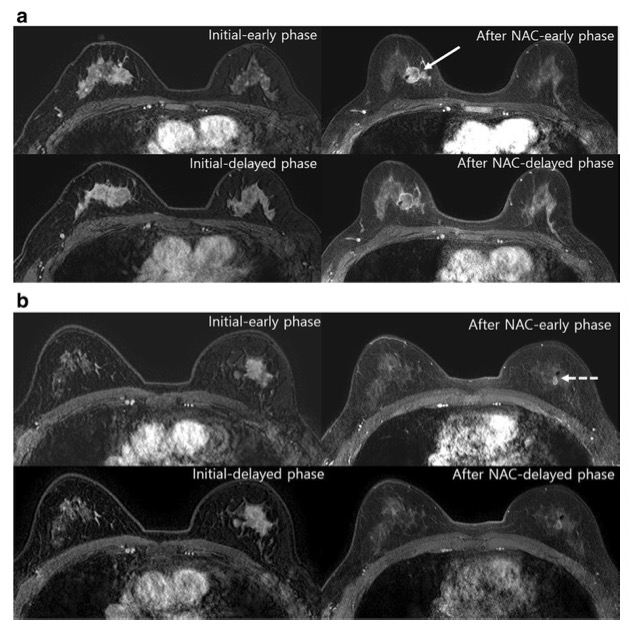
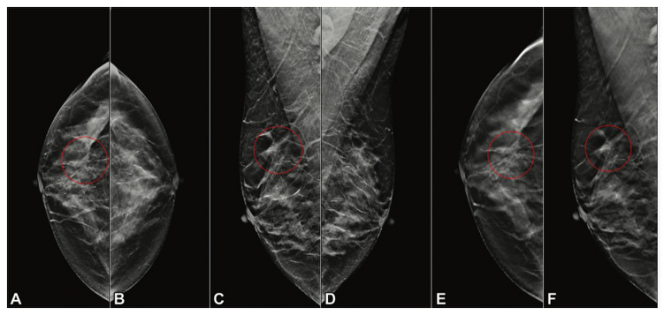
两治疗组的无侵袭性疾病生存率、远处无病生存率和总生存率
三联组和二联组的5年生存率分别是98%和87%(风险比[HR] 0.32,p=0.15);无复发生存率分别是98%和89%(HR 0.41, p=0.25);无局部复发生存率分别是100%和95%(HR 0.41, p=0.43);远处无病生存率分别是98%和92%(HR 0.35, p=0.36);总生存率分别是98%和94%(HR 0.41,p=0.43)。病理完全缓解率与无侵袭性疾病生存率提高相关(HR 0.14, p=0.011)。两治疗组各有一例病理完全缓解后的无侵袭性疾病生存事件。
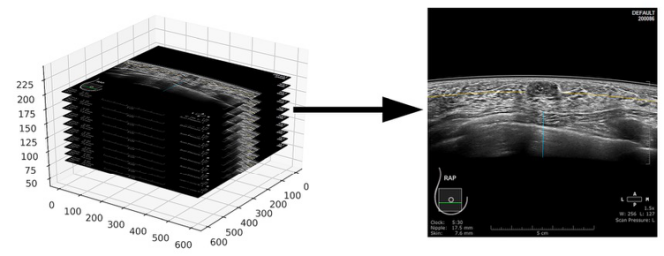
有无病理完全缓解患者的无侵袭性疾病生存率
总之,该研究结果显示,曲妥珠单抗+帕妥珠单抗±紫杉醇治疗12周后获得病理完全缓解的患者可获得很好的生存率。省略进一步化疗并不影响病理完全缓解患者的无侵袭性疾病生存期。
原始出处:
Nitz Ulrike,Gluz Oleg,Graeser Monika et al. De-escalated neoadjuvant pertuzumab plus trastuzumab therapy with or without weekly paclitaxel in HER2-positive, hormone receptor-negative, early breast cancer (WSG-ADAPT-HER2+/HR-): survival outcomes from a multicentre, open-label, randomised, phase 2 trial.[J] .Lancet Oncol, 2022, https://doi.org/10.1016/S1470-2045(22)00159-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Lancet#
39
#Oncol#
40
#曲妥珠#
48
了解一下
67
***
71
lancet上果然牛,感谢梅斯更新及时
44