胸部HRCT对特发性肺动脉高压患者生存的预测价值
2021-11-20 刘少飞 MedSci原创
迄今为止,很少有人关注特发性肺动脉高压(IPAH)患者的胸部高分辨率计算机断层扫描 (HRCT) 发现,而一些小型研究表明,肺部扫描中存在小叶中心磨玻璃影 (GGO) 可能一个显着的负面预后价值。

肺动脉高压 (PH) 定义为静息时平均肺动脉压 (PAPm) 增加 ≥ 25 mmHg,根据右心导管插入术 (RHC) 的评估;最近提出了 20 mmHg 的阈值。有多种与 PH 相关的临床病症,PH 的分类是根据其病理生理机制、临床表现、血流动力学特征和治疗管理的相似性而创建的。
PH 主要有五类:
- 肺动脉高压 (PAH),
- 2左心疾病引起的 PH,
- 肺部疾病和/或缺氧引起的 PH,
- 肺动脉阻塞引起的 PH,
- PH具有不明确和/或多因素的机制。
每个组进一步分为子组。第 1 组,即 PAH,主要由涉及肺动脉、小动脉、毛细血管和小静脉的肺血管疾病引起。肺血管的血管收缩和重塑导致肺血管阻力(PVR)升高,进而导致 PAP 增加,最终对右心室的性能和结构产生不利影响,导致其衰竭。PAH 组包括以下亚型:特发性 (I)PAH、遗传性 (H)PAH、药物和毒素诱导的 PAH、与以下相关的 PAH:结缔组织病、人类免疫缺陷病毒 (HIV) 感染、门脉高压、先天性心脏病或血吸虫病、对钙通道阻滞剂有长期反应的 PAH、具有明显静脉/毛细血管受累特征的 PAH,以及新生儿综合征的最终持续 PH。
尽管广为人知,但尚未对 IPAH 中不均匀肺衰减的现象进行彻底调查和描述。因此,我们研究的目标是:评估 GGO 在 IPAH 中的频率和临床意义,并验证它是否具有参考 ESC/ERS 多维风险评估工具的附加预后价值。
研究方法:
回顾性分析了 1997 年-2011 年间在我院诊断为 IPAH 且可进行胸部 HRCT 扫描的患者。IPAH 的诊断基于 RHC 上 PAH 的证据和排除 PH 的已知原因。所有纳入的患者的 PAPm ≥ 25 mmHg,PAWP ≤ 15 mmHg,PVR > 3 Wood 单位。所有患者都接受了广泛的 PH 差异检查。它包括涵盖个人和家族病史、接触药物和毒素的病历,以及体检结果和其他测试。超声心动图和RHC(正常PAWP)排除左心疾病和先天性心脏病,肺功能检查和HRCT扫描排除肺部疾病,肺动脉增强CT和灌注肺显像排除肺动脉阻塞. 所有患者均排除结缔组织病,HIV 感染检测阴性,门静脉高压症腹部超声检查阴性。其中两名患者有不清楚的 PH 家族史。研究组不包含临床高度怀疑 PVOD/PCH 的患者,即 具有胸部 HRCT 特征三联征的患者,或因血管扩张剂而出现肺充血的患者。然而,没有进行组织病理学验证或基因检测,因此该队列可能包括 PVOD/PCH 过程中患有 HPAH 或 PAH 的患者。
研究结果:
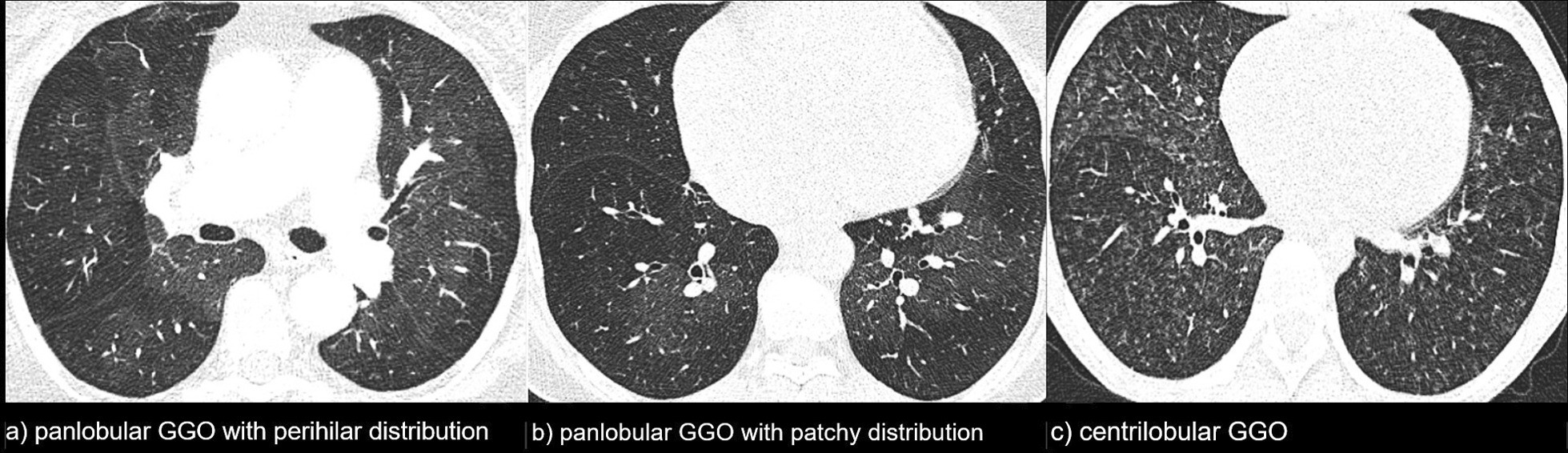
研究组由 110 名 IPAH 患者组成:102 名 (93%) 发病,80 名 (73%) 女性,年龄中位数为 44.3 岁(范围 17.3-78.5 岁)。50 (46%) 名患者在 HRCT 扫描中发现异常肺模式。在 26 (24%) 名患者中发现了 pGGO,其中 50% 的患者出现了肺门周围定位。在 24 名 (22%) 患者中发现了 cGGO,结节广泛存在,并且在所有病例中都没有特定的区域优势。其余 54% 的患者被归类为正常 HRCT 模式。一名 pGGO 患者有淋巴结肿大和间隔增厚。在 cGGO 患者中,2 例有淋巴结肿大,1 例有间隔增厚。三名正常模式的患者有淋巴结病。
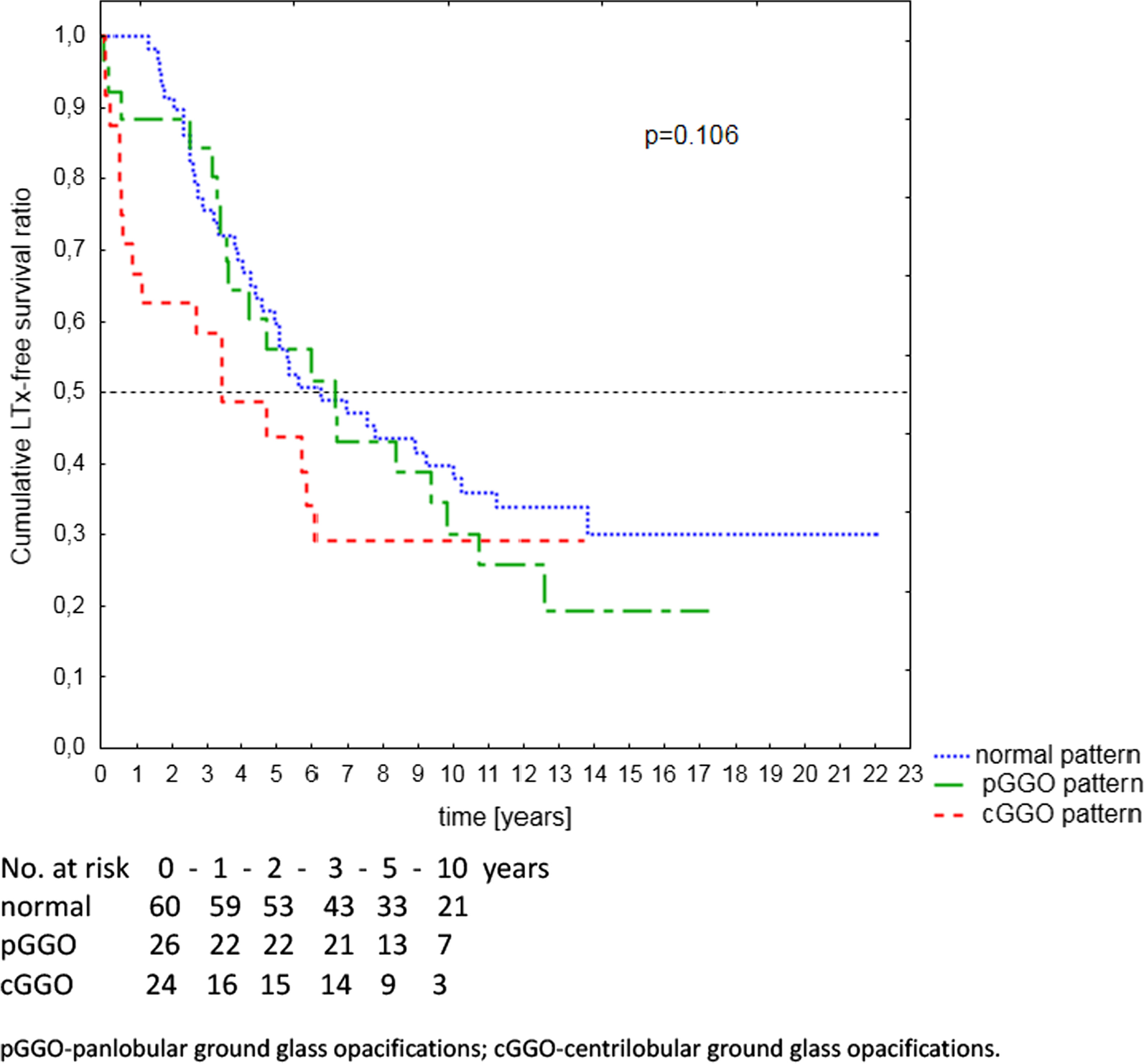
生存及预后
中位随访时间为 5.0 年,范围为 0.1-22.1 年。在此期间,73 名 (66%) 患者死亡(65 名患者)或接受了 LTx(8 名患者),26 名(24%)患者在研究结束时仍然存活,11 名(10%)患者失访. 取决于肺 HRCT 模式的患者的无 LTx 存活率如图2所示, 并总结在表4 中。cGGO 组的中位无 LTx 生存期最低:pGGO 和正常模式组分别为 3.4 年、6.2 年和 5.8 年。在第一年内,cGGO、pGGO 和正常组中所有死亡/LTx 的发生率分别为 50%、15% 和 0%。cGGO 组中 56% 的不利事件发生在前 2 年。
研究结论:
在 46% 的 IPAH 患者中发现 GGO:24% 为 pGGO,22% 为 cGGO。pGGO 的独立预测因子是:阳性咯血史、低风险因素较多和心输出量较低。cGGO 的独立预测因素是:咯血阳性史、年龄较小、右心房压较高和混合静脉血氧饱和度较高。从 2 年的角度来看,CGGO 对结果有负面的预后价值。从长远来看,这种效果没有出现,可能是由于 cGGO 患者的生存期短。肺 HRCT 在 IPAH 中具有重要的独立预后信息,对于扫描中存在 cGGO 的患者,应考虑尽早转诊至肺移植中心。
参考文献:
Kacprzak A, Burakowska B, Kurzyna M, Fijałkowska A, Florczyk M, Wieteska-Miłek M, Darocha S, Torbicki A, Szturmowicz M. Predictive value of chest HRCT for survival in idiopathic pulmonary arterial hypertension. Respir Res. 2021 Nov 17;22(1):293. doi: 10.1186/s12931-021-01893-8. PMID: 34789251.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#特发性#
38
#动脉高压#
34
#患者生存#
36
#肺动脉高压患者#
0
#特发性肺动脉高压#
52
很好的研究
57
很好的办法。
53
#预测价值#
29