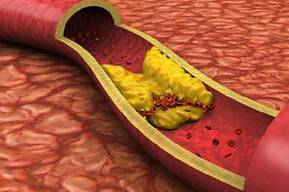
BMJ Open:中国中老年人心血管健康分数及动脉粥样硬化进展的改变
2015-09-18 MedSci MedSci原创
目的:美国心脏病协会(AHA)提出了四种心血管健康行为和3种健康因子的定义。基于这七个指标的心血管健康分数(CHS),评估了个人心血管健康状态的变化。这篇研究的主要目的是调查中老年人不同时间点CHS的改变是否与动脉粥样硬化的进展相关。实验设计:中国前瞻性队列研究方法:根据CHS的变化分为8组(≤-4, -3, -2, -1, 0, 1, 2 和 ≥3)。分析CHS的变化对臂踝脉搏波传导速度(baP
目的:美国心脏病协会(AHA)提出了四种心血管健康行为和3种健康因子的定义。基于这七个指标的心血管健康分数(CHS),评估了个人心血管健康状态的变化。这篇研究的主要目的是调查中老年人不同时间点CHS的改变是否与动脉粥样硬化的进展相关。
实验设计:国内前瞻性队列研究
方法:根据CHS的变化分为8组(≤-4, -3, -2, -1, 0, 1, 2 和 ≥3)。分析CHS的变化对臂踝脉搏波传导速度(baPWV)的变化影响,以及对动脉粥样硬化进展的影响。
受试者:共3951名受试者满足纳入标准(大于40岁,无卒中,短暂性脑缺血发作,心肌梗死病史),并且有完整的信息。
结果:随着CHS变化的增加,baPWV变化逐渐减少(分别为126.46±355.91, 78.4±343.81, 69.6±316.27, 49.59±287.57, 57.07±261.17, 40.45±264.27, 37.45±283.26 以及21.66±264.17 cm/s)。多变量线性回归分析表明这两个变量之间呈负相关,校正其他危险因素后,仍呈负相关。CHS每增加一分,baPWV下降15.22 cm/s。
结论:CHS变化与baPWV变化呈负相关,也证实了是中老年人动脉粥样硬化进展的的独立预测因子。
原文出处:
Gao J, Bao M, Liu Y,et al.Changes in cardiovascular health score and atherosclerosis progression in middle-aged and older persons in China: a cohort study. BMJ Open. 2015 Aug 26
方法:根据CHS的变化分为8组(≤-4, -3, -2, -1, 0, 1, 2 和 ≥3)。分析CHS的变化对臂踝脉搏波传导速度(baPWV)的变化影响,以及对动脉粥样硬化进展的影响。
受试者:共3951名受试者满足纳入标准(大于40岁,无卒中,短暂性脑缺血发作,心肌梗死病史),并且有完整的信息。
结果:随着CHS变化的增加,baPWV变化逐渐减少(分别为126.46±355.91, 78.4±343.81, 69.6±316.27, 49.59±287.57, 57.07±261.17, 40.45±264.27, 37.45±283.26 以及21.66±264.17 cm/s)。多变量线性回归分析表明这两个变量之间呈负相关,校正其他危险因素后,仍呈负相关。CHS每增加一分,baPWV下降15.22 cm/s。
结论:CHS变化与baPWV变化呈负相关,也证实了是中老年人动脉粥样硬化进展的的独立预测因子。
原文出处:
Gao J, Bao M, Liu Y,et al.Changes in cardiovascular health score and atherosclerosis progression in middle-aged and older persons in China: a cohort study. BMJ Open. 2015 Aug 26
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#中老年#
24
#BMJ#
26
#PE#
31
#中老年人#
28
#粥样硬化#
25