NEJM:注射cabotegravir方案用于HIV高危人群暴露前预防
2021-08-12 MedSci原创 MedSci原创
在HIV感染高风险人群中,长效注射cabotegravir暴露前预防方案的疗效优于每日口服替诺福韦-恩曲他滨方案,但长效整合酶抑制剂耐药性问题值得关注

尽管HIV预防已获得了显著进步,但全球每日HIV新感染人数仍在5000例以上,目前最主流的暴露前预防(PrEP)手段为口服富马酸替诺福韦-恩曲他滨(TDF-FTC),其效果与剂量和依从性显著相关。长效注射cabotegravir(CAB-LA)是一种整合酶抑制剂,通过臀肌肌肉注射,具有良好的抗HIV活性。近日研究人员考察了CAB-LA作为一种长效HIV暴露前预防手段的前景。

本次研究为一项随机、双盲、非劣效性试验,参与人群为男男同性恋以及变性女人群,参与者每8周肌肉注射一次600 mg的Cabotegravir或每日口服TDF-FTC,随访153周。研究的主要终点是偶发性HIV感染。
4566名参与者,其中570名(12.5%)为变性女性,平均年龄26岁,在第一次预先计划的中期终点分析时,研究因CAB-LA组疗效显著而提前停止。在1698名来自美国的参与者(845名黑人,49.8%)中, 52名参与者发生HIV感染事件,其中cabotegravir组13例(发病率为0.41/100参与者随访年),TDF-FTC组39例(发病率为1.22/100参与者随访年,危险比为0.34),其他亚组的结论与美国亚组一致。Cabotegravir组81.4%的参与者出现注射部位反应。在CAB-LA组HIV感染人群中,存在整合酶抑制剂耐药性和HIV感染检测延迟现象。未发现任何安全问题。

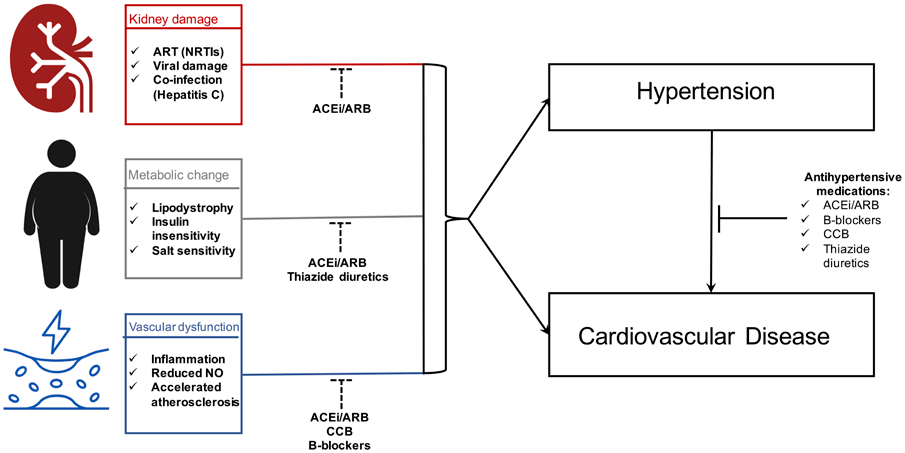
组间HIV感染风险差异
研究认为,在HIV感染高风险人群中,长效注射cabotegravir暴露前预防方案的疗效优于每日口服替诺福韦-恩曲他滨方案,但长效整合酶抑制剂耐药性问题值得关注。
原始出处:
Raphael J. Landovitz et al. Cabotegravir for HIV Prevention in Cisgender Men and Transgender Women. N Engl J Med,August 12,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#高危人群#
35
#Cabotegravir#
0
#ABO#
36
谢谢
62
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
75