Stroke:症状性颈动脉斑块患者以黄嘌呤氧化酶表达增加为特征
2021-06-11 MedSci原创 MedSci原创
黄嘌呤氧化酶(XO)是尿酸代谢的关键酶,被认为是促进动脉粥样硬化斑块进展的氧化途径,但其在斑块不稳定性中的作用尚未阐明。巨噬细胞中XO过表达与血清尿酸升高和高密度脂蛋白胆固醇水平降低相关。
黄嘌呤氧化酶(XO)是尿酸代谢的关键酶,被认为是促进动脉粥样硬化斑块进展的氧化途径,但其在斑块不稳定性中的作用尚未阐明。

近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员假设有症状患者颈动脉斑块中表达XO与心血管危险因素相关。
根据有无症状对患者进行分层,研究人员从44例有症状患者和44例无缺血性脑事件患者中获取颈动脉粥样硬化斑块,并通过免疫组化检测了XO蛋白的表达,并比较各组间XO和CD68(巨噬细胞标志物)表达的细胞百分比。研究人员对参与者的生化和人口统计学心脏代谢危险因素也进行了测量。
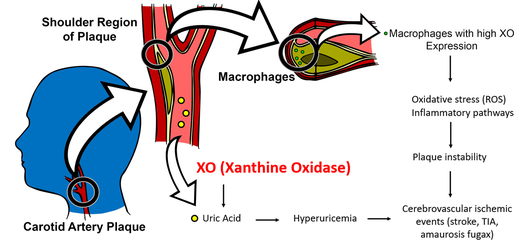
与无症状斑块患者相比,有症状患者的颈动脉粥样硬化斑块与XO表达增高显著相关(中位数[四分位数范围]:1.24 [2.09] vs 0.16 [0.34];P<0.001),且循环中尿酸水平显著升高(平均±SD: 7.36±2.10 vs 5.37±1.79 mg/dL;P<0.001)。此外,颈动脉粥样硬化斑块中XO表达与血清高密度脂蛋白胆固醇水平呈负相关(P=0.010, r=−0.30),与循环尿酸水平直接相关(P<0.001, r=0.45)。在有症状患者斑块中表达XO的巨噬细胞的平均百分比显著高于无症状患者的斑块(中位数[四分位数范围]:93.37% [25] vs 46.15% [21];P<0.001)。
由此可见,巨噬细胞中XO过表达与血清尿酸升高和高密度脂蛋白胆固醇水平降低相关,可能在不稳定性颈动脉斑块中具有潜在的作用。
原始出处:
Morsaleh Ganji.et al.Carotid Plaques From Symptomatic Patients Are Characterized by Local Increase in Xanthine Oxidase Expression.stroke.2021.https://doi.org/10.1161/STROKEAHA.120.032964
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#颈动脉#
28
#黄嘌呤#
48
#颈动脉斑块#
43
#斑块#
0
好文章
61
#酶表达#
39
学习。
46